Understanding Your RDW Blood Test Results
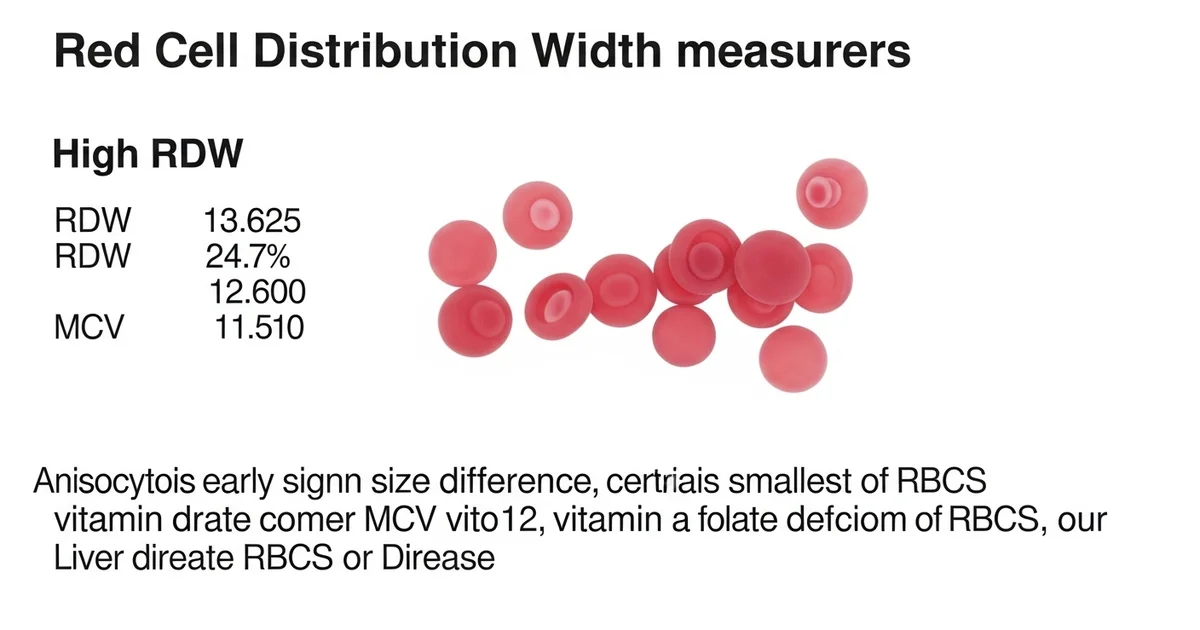
Direct answer: The Red Cell Distribution Width (RDW) blood test measures the variation in the size of your red blood cells (RBCs). A high RDW means there is a significant size difference between your smallest and largest RBCs, a condition called anisocytosis. This can be an early sign of certain medical conditions, such as iron deficiency anemia, vitamin B12 or folate deficiency, or liver disease. It is often interpreted alongside other complete blood count (CBC) results, like the MCV.
TL;DR The Red Cell Distribution Width (RDW) test is a standard part of a complete blood count (CBC) that measures the variation in the size of your red blood cells. While a normal RDW indicates your red blood cells are mostly uniform in size, a high RDW suggests a mix of small and large cells. This variation, known as anisocytosis, can be an important clue for diagnosing various health conditions, often before other symptoms appear. Your doctor will interpret your RDW level in the context of other CBC values, particularly the Mean Corpuscular Volume (MCV), to get a clearer picture of your red blood cell health.
- RDW measures the size variation in your red blood cells, not the actual size.
- A high RDW means your red blood cells vary significantly in size, which can be a sign of a nutritional deficiency (like iron, B12, or folate) or other conditions.
- A low RDW is uncommon and typically not a cause for concern.
- The RDW test is part of a routine complete blood count (CBC) panel.
- Doctors use the RDW along with the MCV (which measures the average cell size) to help narrow down the cause of anemia.
- Conditions like iron deficiency anemia often present with a high RDW and low MCV.
- Other issues, such as liver disease or certain genetic disorders, can also lead to an elevated RDW.
Want the full explanation? Keep reading ↓
RDW Blood Test: Measuring RBC Size Variation
The Red Cell Distribution Width (RDW) is a standard component of a Complete Blood Count (CBC), one of the most frequently ordered laboratory tests. While other CBC parameters like hemoglobin and hematocrit measure the quantity of red blood cells (RBCs), the RDW provides crucial information about their quality—specifically, the variation in their size. This measurement, known as anisocytosis, is a key indicator of how effectively your bone marrow is producing red blood cells.
Interpreting the RDW is not about a single "good" or "bad" number. Instead, its clinical value shines when evaluated alongside other CBC indices, particularly the Mean Corpuscular Volume (MCV), which measures the average size of your red blood cells. Together, these markers help clinicians classify different types of anemia and can even offer prognostic insights into a wide range of medical conditions.
What Does RDW Measure? Understanding Anisocytosis
The RDW test quantifies the variability in the volume and size of your circulating red blood cells. In a healthy state, red blood cells are produced in a relatively uniform, biconcave disc shape, roughly 6-8 micrometers in diameter. A low RDW reflects this uniformity.
When the RDW is elevated, it signifies a high degree of variation in RBC size, a condition called anisocytosis. This suggests that something is disrupting the normal, orderly production of red blood cells in the bone marrow. Imagine a factory producing identical parts; if the machinery malfunctions, it might start producing parts of varying sizes. Similarly, an elevated RDW signals a potential issue with RBC production.
There are two primary ways RDW is reported on a lab report:
- RDW-CV (%): This is the most common method. It is the coefficient of variation of RBC volume, calculated using the standard deviation of RBC volume and the MCV. It is expressed as a percentage.
- RDW-SD (fL): This is the standard deviation of RBC volume, measured directly in femtoliters (fL). It is an actual measurement of the width of the RBC size distribution curve and is not influenced by the average cell size (MCV).
Is Your RDW Normal? Reference Ranges Explained
Understanding the typical range for RDW is the first step in interpreting your results. However, it's crucial to remember that these ranges can vary slightly depending on the laboratory and the specific analyzer used. Always compare your results to the reference range provided on your lab report.
| Population | Normal Range (RDW-CV) | Units | Notes |
|---|---|---|---|
| Adults | ~11.5% to 15.0% | % | This is a general range; some labs may use up to 15.5%. |
| Newborns | ~14.9% to 18.7% | % | RDW is naturally higher in newborns and decreases during infancy. |
| RDW-SD | ~35 fL to 56 fL | fL | This is a direct measurement and may be reported instead of RDW-CV. |
Why Is My RDW High? Exploring the Causes of Increased RBC Size Variation
An elevated RDW, or anisocytosis, is a common laboratory finding that serves as a red flag for underlying health issues. It is one of the earliest and most sensitive indicators of problems with red blood cell production, often becoming abnormal before other markers like MCV change. The most frequent causes are related to nutritional deficiencies that impair the bone marrow's ability to create uniform red blood cells.
Nutritional Deficiencies: The Most Common Culprit
The building blocks for healthy red blood cells include iron, vitamin B12, and folate. A deficiency in any of these key nutrients can lead to disordered RBC production and a high RDW.
- Iron Deficiency: This is the classic and most common cause of a high RDW. When iron is scarce, the bone marrow cannot produce enough hemoglobin. This results in the creation of smaller-than-normal red blood cells (microcytes). As the deficiency progresses, there is a mix of newly formed small cells and older normal-sized cells, dramatically increasing the size variation and thus the RDW.
- Vitamin B12 Deficiency: Vitamin B12 is essential for DNA synthesis, which is critical for cell division in the bone marrow. A lack of B12 leads to the production of abnormally large, immature red blood cells (macrocytes). The presence of these large cells alongside any remaining normal cells causes a high RDW.
- Folate (Vitamin B9) Deficiency: Similar to vitamin B12, folate is also vital for DNA synthesis. A deficiency has the same effect, leading to macrocytic anemia and an elevated RDW due to the presence of large, dysfunctional red blood cells.
Anemia and Bone Marrow Disorders
Beyond simple nutritional shortages, a high RDW can signal more complex types of anemia or intrinsic problems with the bone marrow itself.
- Anemia of Chronic Disease/Inflammation (ACD): Long-term inflammatory conditions (like rheumatoid arthritis, IBD, or chronic infections) can interfere with iron utilization and suppress RBC production. This often leads to a high RDW as the bone marrow's function becomes disordered.
- Myelodysplastic Syndromes (MDS): These are a group of cancers where the bone marrow fails to produce enough healthy blood cells. The production that does occur is highly abnormal and dysplastic, often resulting in a very high RDW.
- Sideroblastic Anemia: In this condition, the body has adequate iron but cannot incorporate it into hemoglobin properly. This leads to a "dimorphic" population of RBCs—some are normal, and some are small and pale—causing a significant increase in RDW.
- Hemolytic Anemia: This involves the premature destruction of red blood cells. To compensate, the bone marrow ramps up production and releases large, immature RBCs called reticulocytes. This mixture of normal cells and large new cells increases the RDW.
Other Potential Causes of High RDW
Several other situations can lead to a mix of different-sized red blood cells in circulation.
- Recent Blood Transfusion: A transfusion introduces a population of donor red blood cells. The mix of the recipient's cells and the donor's cells will naturally have different size characteristics, temporarily increasing the RDW.
- Chronic Liver Disease: The liver plays a role in maintaining the health of red blood cell membranes. Severe liver disease can lead to abnormally shaped cells (acanthocytes) and changes in cell volume, which can increase the RDW.
- Alcohol Use Disorder: Excessive alcohol consumption is directly toxic to the bone marrow and can also lead to nutritional deficiencies (especially folate), both of which can result in a high RDW.
What Does It Mean If My RDW Is Low? Understanding Uniform RBC Size
A low RDW is an uncommon finding and is rarely a cause for clinical concern. It simply indicates that your red blood cells are exceptionally uniform in size, with very little variation.
There is no disease or disorder directly associated with a low RDW. While it may occasionally be noted in certain conditions where red blood cell production is uniformly suppressed (like some cases of aplastic anemia) or uniformly abnormal (like some thalassemia traits), it is not used as a diagnostic marker. In most cases, a low RDW in an otherwise healthy individual is considered a normal variant.
How Is RDW Used with MCV? The Power of Combined Interpretation
The true diagnostic power of RDW is unlocked when it is interpreted in conjunction with the Mean Corpuscular Volume (MCV). The MCV tells you the average size of your red blood cells, while the RDW tells you the variation in their size. Combining these two parameters allows for a much more precise classification of anemia.
Interpreting RDW and MCV Together
This table provides a simplified guide for interpreting common RDW and MCV combinations. This is a starting point for a diagnostic investigation, not a final diagnosis.
| RDW | MCV | Common Clinical Possibilities |
|---|---|---|
| High | Low | Suggests a microcytic anemia with high size variation. Classic for iron deficiency anemia. Also seen in RBC fragmentation. |
| High | Normal | Suggests a mixed population of small and large cells that average out to normal. Can indicate early iron/B12/folate deficiency, mixed-cause anemia, or anemia of chronic disease. |
| High | High | Suggests a macrocytic anemia with high size variation. Classic for vitamin B12 or folate deficiency anemia. Also seen in autoimmune hemolytic anemia or myelodysplastic syndrome. |
| Normal | Low | Suggests a uniform population of small cells. Common in anemia of chronic disease and thalassemia trait. |
| Normal | Normal | Suggests a uniform population of normal-sized cells. Can be seen in a healthy person, or in conditions like acute blood loss or aplastic anemia where the cells produced are normal but insufficient in number. |
| Normal | High | Suggests a uniform population of large cells. Can be seen in aplastic anemia, chronic liver disease, or with certain medications (e.g., chemotherapy). |
RDW as a Prognostic Marker: What Else Can It Tell Us?
In recent years, research has highlighted the RDW's role not just in diagnosing anemia, but also as a powerful, independent predictor of outcomes in a wide variety of diseases. A high RDW is increasingly recognized as a general marker of underlying physiological stress, inflammation, and poor health status.
RDW in Cardiovascular Disease
A consistently elevated RDW is strongly associated with worse outcomes in patients with cardiovascular conditions.
- Heart Failure: Patients with heart failure and a high RDW have a significantly higher risk of hospitalization and mortality compared to those with a normal RDW.
- Coronary Artery Disease: In individuals who have had a heart attack (myocardial infarction), a high RDW is a predictor of future adverse cardiac events.
- Atrial Fibrillation: Elevated RDW is linked to an increased risk of stroke in patients with atrial fibrillation.
The exact mechanism is not fully understood but is thought to be related to chronic inflammation, oxidative stress, and poor nutritional status, all of which can affect both red blood cell health and cardiovascular function.
RDW in Other Conditions
The prognostic value of RDW extends to many other areas of medicine.
- Infection and Sepsis: In the intensive care unit (ICU), a rising RDW is a strong predictor of mortality in patients with sepsis.
- Cancer: Many studies have shown that a high RDW at the time of cancer diagnosis is associated with more advanced stage disease and poorer survival rates across various cancer types, including colon, lung, and breast cancer.
- Liver and Kidney Disease: In patients with chronic liver or kidney disease, a higher RDW is linked to disease severity and a greater risk of complications.
- Overall Mortality: Even in the general population, a high RDW has been shown to be a robust predictor of all-cause mortality, suggesting it reflects an individual's overall health and physiological resilience.
What Are the Next Steps for an Abnormal RDW?
An abnormal RDW is not a diagnosis in itself but a clue that warrants further investigation. Your healthcare provider will use this result as a guide for what to do next.
Checklist for Follow-Up on an Abnormal RDW:
- Review the Entire CBC: The first step is to analyze the RDW in the context of the MCV, hemoglobin, hematocrit, and RBC count. This helps classify the potential type of anemia.
- Evaluate for Nutritional Deficiencies: If a high RDW is present, especially with a low or high MCV, your doctor will likely order tests to check for deficiencies.
- Iron Studies: Ferritin, serum iron, TIBC (total iron-binding capacity), and transferrin saturation.
- Vitamin Levels: Serum vitamin B12 and folate levels.
- Assess for Inflammation: If anemia of chronic disease is suspected, your provider may order inflammatory markers.
- C-Reactive Protein (CRP)
- Erythrocyte Sedimentation Rate (ESR)
- Consider Other Tests: Depending on the clinical picture, other tests may be necessary.
- Reticulocyte Count: Measures the production of new red blood cells.
- Peripheral Blood Smear: A microscopic examination of the blood to look at the shape and size of blood cells directly.
- Hemoglobin Electrophoresis: Used to diagnose thalassemia and other hemoglobinopathies.
- Bone Marrow Biopsy: Considered if a serious bone marrow disorder like MDS or aplastic anemia is suspected.
Frequently Asked Questions
What is the most common cause of abnormal Red Cell Distribution Width (RDW) levels?
The single most common cause of a high RDW is iron deficiency anemia. In the early stages of iron deficiency, the bone marrow begins to produce smaller red blood cells (microcytes) while older, normal-sized cells are still in circulation. This mixture of small and normal cells creates significant size variation, causing the RDW to increase. In fact, the RDW is often the very first marker in a CBC to become abnormal in developing iron deficiency, sometimes even before hemoglobin levels drop or the MCV becomes low. Other common causes include vitamin B12 and folate deficiencies. An abnormally low RDW is very rare and is generally not considered clinically significant.
How often should I get my Red Cell Distribution Width (RDW) tested?
The RDW is not typically tested as a standalone marker. It is a standard component of the Complete Blood Count (CBC), which is a routine test. The frequency of testing depends on your overall health status:
- Healthy Individuals: For a healthy adult with no symptoms, a CBC (including RDW) may be ordered as part of a routine physical exam, perhaps every few years, though this varies by clinical practice.
- Monitoring a Condition: If you are being treated for a condition known to cause an abnormal RDW (like iron deficiency anemia), your provider may order a CBC more frequently (e.g., every few months) to monitor your response to treatment.
- Symptomatic Patients: If you present with symptoms like fatigue, weakness, shortness of breath, or paleness, your doctor will almost certainly order a CBC immediately to investigate the cause.
Can lifestyle changes improve my Red Cell Distribution Width (RDW) levels?
Yes, lifestyle changes can improve your RDW, particularly if the elevation is caused by nutritional deficiencies. If your high RDW is due to a lack of iron, vitamin B12, or folate, addressing these shortages through diet and supplementation is the primary way to normalize it.
- For Iron Deficiency: Increase your intake of iron-rich foods like red meat, poultry, fish, lentils, beans, spinach, and fortified cereals. Consuming vitamin C (e.g., from citrus fruits) with iron-rich meals can enhance absorption.
- For B12/Folate Deficiency: Increase your intake of foods rich in these vitamins. Folate is found in leafy green vegetables, fruits, and beans. Vitamin B12 is primarily found in animal products like meat, dairy, and eggs.
- Reducing Alcohol Intake: If excessive alcohol consumption is a contributing factor, reducing or eliminating alcohol can allow the bone marrow to recover and improve RBC production, thereby normalizing the RDW.
It is essential to consult with a healthcare provider before starting any new supplement regimen. They can confirm the deficiency with specific tests and recommend the appropriate dosage, as correcting an abnormal RDW depends on successfully treating its underlying cause.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.