Understanding Your White Blood Cell Count Results
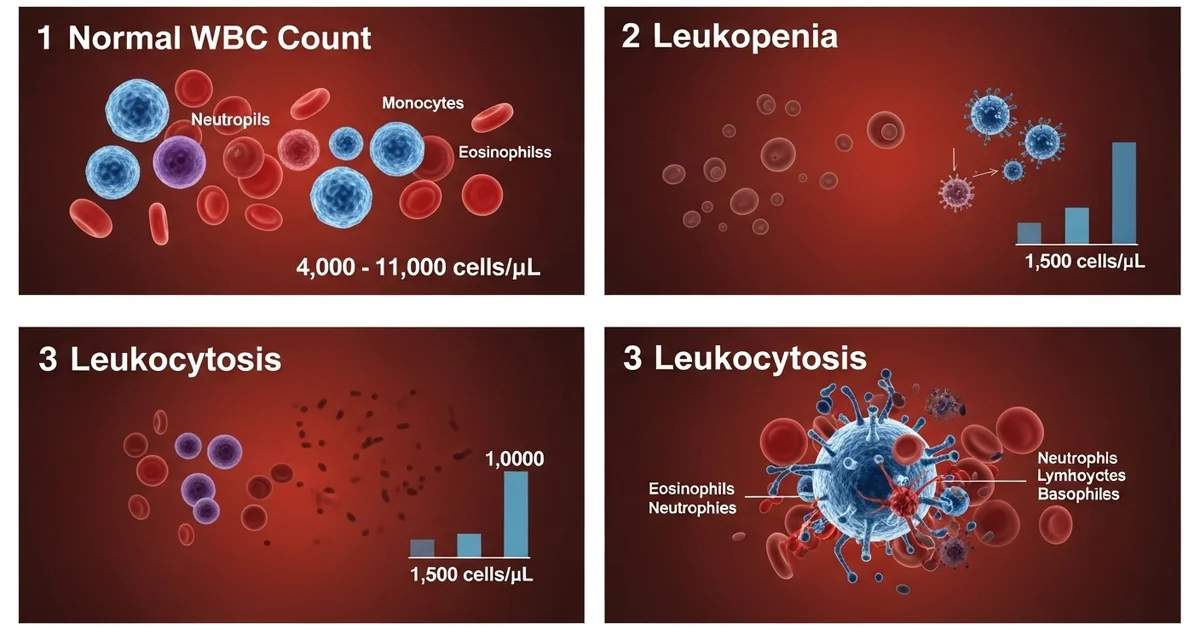
Direct answer: A normal white blood cell (WBC) count for adults is typically between 4,000 and 11,000 cells per microliter of blood. A count below this range is called leukopenia, which can increase infection risk. A count above this range is called leukocytosis, often indicating your body is fighting an infection or inflammation. Your specific lab's reference range may vary slightly. Always discuss your results with a healthcare provider to understand what they mean for your personal health.
TL;DR Your white blood cell (WBC) count is a key part of a complete blood count (CBC) test that measures the number of infection-fighting cells in your body. Understanding whether your count is high, low, or normal is crucial for assessing your immune health. A normal range is generally considered to be 4,000 to 11,000 cells/mcL, but this can vary by age and the specific lab.
What is a WBC Count? It measures the total number of white blood cells, which are essential components of your immune system that help fight off infections and other diseases.
Normal WBC Range: For most adults, a healthy range is between 4,000 and 11,000 white blood cells per microliter (cells/mcL) of blood.
Leukopenia (Low WBC Count): A count below 4,000 cells/mcL is considered low. This condition, known as leukopenia, can weaken your immune system, making you more susceptible to infections. It can be caused by autoimmune disorders, bone marrow problems, or certain medications.
Leukocytosis (High WBC Count): A count above 11,000 cells/mcL is considered high. This is called leukocytosis and is most often a sign that your body is fighting an infection or dealing with inflammation. It can also be linked to stress, certain drugs, or more serious conditions like leukemia.
Why It Matters: Abnormal WBC levels don't always signal a serious problem, but they are an important indicator that requires further investigation. Your doctor will interpret the results in the context of your overall health and other lab tests.
Next Steps: Never interpret your lab results alone. Always consult with your healthcare provider to understand the cause of an abnormal WBC count and determine the appropriate next steps for diagnosis or treatment.
Want the full explanation? Keep reading ↓
What is a Healthy White Blood Cell Count?
Your White Blood Cell (WBC) count is a fundamental health marker that measures the total number of immune cells in your blood. As a key component of the Complete Blood Count (CBC) test, it provides a crucial snapshot of your body's ability to fight infection, inflammation, and disease. Understanding your WBC count is the first step in assessing the strength of your immune defenses.
A normal WBC count indicates that your immune system is likely functioning as expected. However, these ranges are not absolute and can be influenced by factors like age, time of day, and even stress levels. For a more in-depth look at what these cells do, learning about the [different types of white blood cells and their roles] can provide valuable context for your lab results.
Reference ranges can vary slightly between laboratories, but the following table provides generally accepted values for different populations. It is essential to compare your results to the specific range provided by the lab that performed your test.
Normal White Blood Cell (WBC) Reference Ranges
| Population | Normal Range (cells/mcL) | Units | Notes |
|---|---|---|---|
| Adults | 4,000 - 11,000 | cells/mcL | Can vary based on lab, time of day, and physical stress. |
| Children (1-10 years) | 4,500 - 13,500 | cells/mcL | Ranges are higher than adults and decrease steadily with age. |
| Newborns (<1 month) | 9,000 - 30,000 | cells/mcL | Very high at birth; changes rapidly in the first few weeks of life. |
Worried About a High WBC Count? Understanding Leukocytosis
Leukocytosis is the medical term for a white blood cell count that is higher than the normal reference range, typically above 11,000 cells/mcL in adults. While a high count can be alarming, it is most often a sign that your immune system is actively working to fight off an invader or respond to inflammation. It's your body's natural and appropriate defense mechanism.
However, a persistently or extremely high WBC count can also signal a more serious underlying condition that requires medical investigation. The key is to determine why your body is producing so many white blood cells.
What Causes a High White Blood Cell Count?
The causes of leukocytosis are broad, ranging from common infections to chronic diseases. A healthcare provider will interpret your high WBC count in the context of your overall health, symptoms, and other lab results.
Common Causes of Leukocytosis:
- Infections: This is the most frequent cause. Both bacterial (e.g., strep throat, pneumonia, UTIs) and viral (e.g., mononucleosis) infections trigger the bone marrow to release more WBCs.
- Inflammation: Chronic inflammatory conditions like rheumatoid arthritis, inflammatory bowel disease (IBD), or vasculitis can lead to a consistently elevated WBC count.
- Tissue Damage: Trauma from burns, surgery, or a heart attack causes an inflammatory response that elevates WBCs.
- Severe Allergic Reactions: Conditions like anaphylaxis can cause a spike in certain types of WBCs, particularly eosinophils.
- Medications: Some drugs are known to increase WBC production, including corticosteroids (like prednisone), lithium, and certain asthma medications (beta-agonists).
Serious Causes of Leukocytosis:
- Bone Marrow Disorders: Conditions like myeloproliferative neoplasms cause the bone marrow to overproduce one or more types of blood cells, leading to very high counts.
- Leukemia: Cancers of the blood-forming tissues, such as Acute Myeloid Leukemia (AML) or Chronic Lymphocytic Leukemia (CLL), result in the uncontrolled production of abnormal white blood cells.
- Solid Tumors: Some cancers, particularly lung cancer, can produce hormone-like substances that stimulate the bone marrow to produce more WBCs.
Feeling Unwell? Symptoms Associated with Leukocytosis
The symptoms of leukocytosis are often the symptoms of the underlying cause, not the high WBC count itself. For example, if an infection is the cause, you may experience fever and fatigue.
Common Symptoms to Watch For:
- Fever and chills: Classic signs of infection.
- Body aches and fatigue: General feelings of being unwell (malaise).
- Localized pain, redness, or swelling: Indicates a specific site of infection or inflammation.
- Difficulty breathing or coughing: May suggest a respiratory infection like pneumonia.
In rare cases of extremely high WBC counts (hyperleukocytosis, often >100,000 cells/mcL), the blood can become too thick, leading to serious symptoms like stroke, vision changes, or respiratory distress. This is a medical emergency.
What Happens After a High WBC Result?
A single high WBC reading is not a diagnosis. Your doctor will use it as a starting point for further investigation.
Next Steps May Include:
- Reviewing Your History: Your provider will ask about recent illnesses, medications, and any existing health conditions.
- Performing a Physical Exam: To look for signs of infection or inflammation.
- Ordering a WBC Differential: This crucial test breaks down the [WBC count into its specific cell types] (neutrophils, lymphocytes, etc.). Identifying which type is elevated provides vital clues to the cause. For instance, high neutrophils suggest a bacterial infection, while high lymphocytes point toward a viral infection.
- Additional Blood Tests: Markers of inflammation like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may be ordered.
- Imaging: An X-ray or CT scan may be needed to locate a suspected infection or tumor.
- Bone Marrow Biopsy: If a primary blood disorder or leukemia is suspected, this procedure is the definitive diagnostic test.
Concerned About a Low WBC Count? Understanding Leukopenia
Leukopenia is the medical term for a white blood cell count that is below the normal reference range, typically under 4,000 cells/mcL in adults. This condition indicates a weakened immune system, which can leave you more vulnerable to infections.
While a slightly low count may be temporary and resolve on its own, a significantly or persistently low count requires prompt medical evaluation to identify the cause and prevent complications. The severity of leukopenia depends on how low the count is and which specific type of white blood cell is affected.
What Causes a Low White Blood Cell Count?
Leukopenia occurs when the body either isn't producing enough white blood cells in the bone marrow or when existing cells are being destroyed faster than they can be replaced.
Key Causes of Leukopenia:
- Viral Infections: Many viruses can temporarily suppress bone marrow function, including the flu, mononucleosis (mono), measles, and HIV.
- Cancer Treatments: Chemotherapy and radiation therapy are designed to kill rapidly dividing cells. Because blood cells are produced rapidly, these treatments are a very common cause of severe leukopenia.
- Bone Marrow Diseases:
- Aplastic Anemia: The bone marrow fails to produce enough of all three types of blood cells (red, white, and platelets).
- Myelodysplastic Syndromes (MDS): A group of disorders where the bone marrow produces abnormal, ineffective blood cells.
- Leukemia: While some leukemias cause high WBC counts, others can crowd out normal bone marrow function, leading to low counts.
- Autoimmune Disorders: Conditions like lupus (SLE) and rheumatoid arthritis can cause the immune system to mistakenly attack and destroy its own white blood cells.
- Severe Infections: Overwhelming bacterial infections (sepsis) can sometimes deplete the body's supply of WBCs.
- Medications: A wide range of drugs can suppress WBC production, including some antibiotics, diuretics, antipsychotics, and immunosuppressants used for organ transplants.
- Nutritional Deficiencies: Severe, long-term deficiencies in vitamin B12, folate, or copper can impair the bone marrow's ability to produce cells.
Are You at Risk? Symptoms of Leukopenia
Mild leukopenia often causes no symptoms at all and may only be discovered on a routine blood test. When symptoms do appear, they are usually the result of an infection that the body is struggling to fight.
Symptoms of a Weakened Immune System:
- Frequent or recurring infections
- Fever and chills
- Mouth sores or ulcers
- Sore throat and persistent cough
- Skin infections, rashes, or abscesses
- Unusual fatigue and weakness
The most dangerous form of leukopenia is neutropenia, a low count of neutrophils. Since neutrophils are the primary defense against bacterial infections, severe neutropenia creates a high risk for life-threatening sepsis.
What Are the Next Steps for a Low WBC Result?
Investigating leukopenia is critical to protecting your health. Your healthcare provider will focus on identifying the underlying cause and assessing your risk of infection.
Diagnostic and Management Steps:
- Detailed Medication Review: Your doctor will carefully review all prescription, over-the-counter, and supplement use, as medications are a common cause.
- WBC Differential: As with leukocytosis, a differential is essential to determine which cell line is low (e.g., neutropenia, lymphopenia). This helps narrow down the potential causes.
- Testing for Infections: Blood cultures and tests for specific viruses like EBV (mono) or HIV may be performed.
- Autoimmune and Nutritional Screening: Blood tests can check for autoantibodies (seen in lupus) and levels of vitamin B12, folate, and copper.
- Bone Marrow Biopsy: If the cause is not apparent or a primary bone marrow disorder is suspected, a biopsy is necessary to directly examine the blood-producing cells.
- Protective Measures: If your count is significantly low, your doctor may advise you on how to avoid infections, such as practicing meticulous hand hygiene, avoiding crowds, and ensuring food is cooked thoroughly. In some cases, growth factor injections (G-CSF) may be used to stimulate WBC production.
Frequently Asked Questions
What is the most common cause of abnormal White Blood Cell Count (WBC) levels?
The most common cause of an abnormal WBC count is a transient infection. A high WBC count (leukocytosis) is frequently caused by a bacterial infection, while a low WBC count (leukopenia) can often be a temporary result of a viral infection, like the common cold or flu. In both cases, the WBC count typically returns to normal after the infection resolves.
How often should I get my White Blood Cell Count (WBC) tested?
For healthy individuals with no symptoms, a WBC count is typically checked as part of a routine physical exam with a Complete Blood Count (CBC), often every 1 to 3 years. If you have a known medical condition that can affect blood cells (like an autoimmune disorder), are undergoing treatments like chemotherapy, or are taking medications known to affect WBCs, your doctor will recommend a much more frequent monitoring schedule. Always follow your healthcare provider's specific advice.
Can lifestyle changes improve my White Blood Cell Count (WBC) levels?
Yes, but only to a certain extent and primarily for maintaining a healthy immune system, not for treating serious medical conditions. A balanced diet rich in vitamins and minerals (especially B12, folate, zinc, and copper) is essential for healthy bone marrow function. Managing stress, getting adequate sleep, and regular moderate exercise can also support a robust immune system. However, lifestyle changes cannot correct severe leukopenia or leukocytosis caused by underlying diseases like leukemia or autoimmune disorders; these require specific medical treatment.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.