Understanding Your White Blood Cells and What They Mean for You
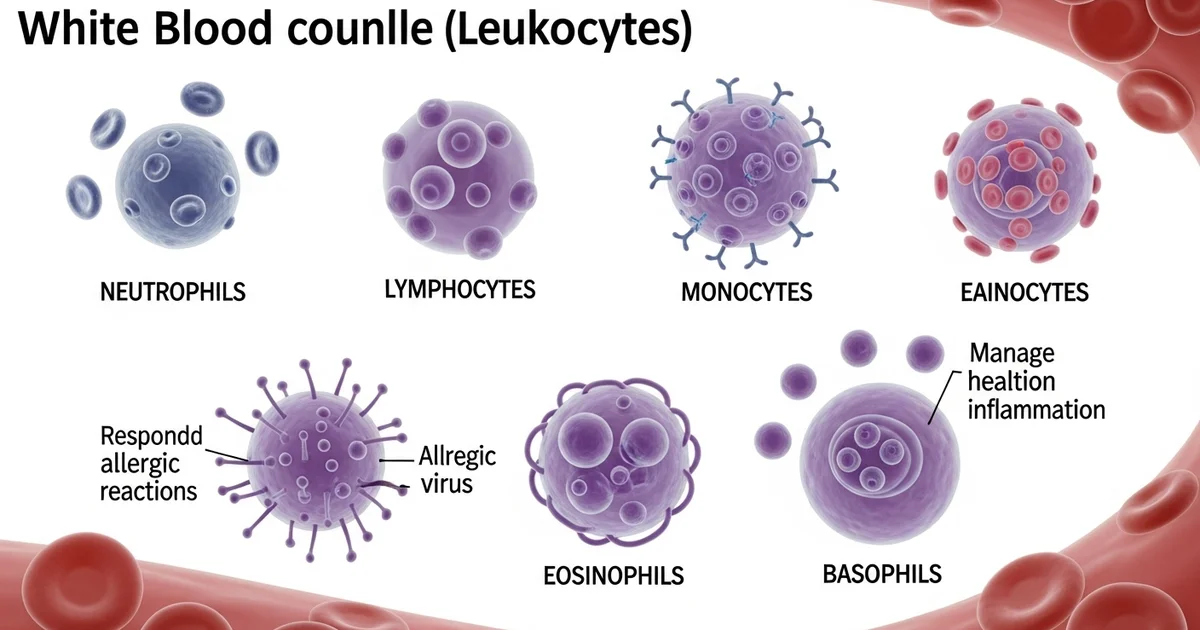
Direct answer: White blood cells (WBCs), or leukocytes, are a key part of your immune system, defending your body against infection and disease. There are five main types: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Each type has a specific role, from fighting bacteria and viruses to responding to allergic reactions and inflammation. A white blood cell count measures the number of these cells in your blood, providing important insights into your overall health.
TL;DR Your white blood cells (WBCs) are essential soldiers in your body's immune system, constantly working to protect you from illness. A complete blood count (CBC) test measures these cells, and understanding the different types can help you make sense of your results. There are five major types of leukocytes, each with a unique and vital job.
- Neutrophils: The most common type, these are your body's first line of defense, rapidly responding to sites of infection to engulf and destroy bacteria and fungi.
- Lymphocytes: These include B-cells, which create antibodies to remember and fight off specific invaders, and T-cells, which directly attack infected cells and regulate the immune response.
- Monocytes: The largest type of WBC, they clean up dead cells and debris. They can also transform into macrophages to break down bacteria and other foreign material.
- Eosinophils: These cells are crucial for combating parasitic infections and are also heavily involved in allergic reactions, like asthma and hay fever.
- Basophils: The least common type, they release histamine and other chemicals during allergic responses and play a role in preventing blood from clotting too quickly.
Together, these cells form a coordinated defense network. An abnormal count in any of these types can signal infection, inflammation, an autoimmune disorder, or other medical conditions, highlighting their importance as indicators of your health.
Want the full explanation? Keep reading ↓
What Are the Main Categories of White Blood Cells?
Your immune system is a complex network of cells and proteins that defend your body against infection. At the heart of this defense force are your white blood cells, also known as leukocytes. While a total [WBC count provides a crucial overview of your immune system's status], understanding the specific types of white blood cells and their unique roles offers a much deeper insight into your health.
Leukocytes are broadly divided into two main categories based on their appearance under a microscope:
- Granulocytes: These cells contain visible granules in their cytoplasm. These granules are sacs filled with powerful enzymes and chemicals that are released to fight off pathogens. The granulocyte family includes neutrophils, eosinophils, and basophils.
- Agranulocytes: These cells lack visible granules. They have a clear cytoplasm and are key players in orchestrating more specific, long-term immune responses. This group includes lymphocytes and monocytes.
A standard lab test called a WBC differential breaks down the percentage of each of these five cell types in your blood, providing a detailed blueprint of your immune activity.
Confused by Your WBC Differential? Understanding the Granulocytes
Granulocytes are the immune system's rapid-response team. They are typically the first to arrive at the scene of an infection or injury, ready to attack invaders and signal for backup. Abnormal levels of any granulocyte can point toward specific health issues, from common infections to chronic inflammatory conditions.
The table below shows the typical reference ranges for each type of white blood cell in a differential count. It's important to remember that these ranges can vary slightly between laboratories.
| Cell Type | Normal Range (Percentage) | Normal Range (Absolute) | Primary Function |
|---|---|---|---|
| Neutrophils | 40% - 60% | 2.0 - 7.0 x 10⁹/L | Fighting bacterial and fungal infections |
| Lymphocytes | 20% - 40% | 1.0 - 3.0 x 10⁹/L | Fighting viral infections, adaptive immunity |
| Monocytes | 2% - 8% | 0.2 - 1.0 x 10⁹/L | Phagocytosis, becoming macrophages |
| Eosinophils | 1% - 4% | 0.02 - 0.5 x 10⁹/L | Fighting parasites, allergic reactions |
| Basophils | 0.5% - 1% | 0.02 - 0.1 x 10⁹/L | Allergic response, releasing histamine |
Neutrophils: Your Body's First Line of Defense
Neutrophils are the most abundant type of white blood cell, making up the bulk of your immune infantry. Their primary job is phagocytosis—engulfing and digesting harmful microorganisms, especially bacteria and fungi. They are the main component of pus, which is why it appears whitish-yellow at the site of an infection.
When your body detects an infection, the bone marrow ramps up neutrophil production. It may even release immature neutrophils, called bands, into the bloodstream. A high number of bands, known as a "left shift," is a strong indicator of an acute, severe infection.
High Neutrophils (Neutrophilia): An elevated neutrophil count is a classic sign that your body is fighting a battle. Common causes include:
- Bacterial infections (e.g., strep throat, pneumonia, urinary tract infections)
- Inflammation from injury, surgery, or chronic conditions like rheumatoid arthritis
- Physical or emotional stress
- Certain medications, such as corticosteroids
- Some types of leukemia, which can cause a [dangerously high white blood cell count].
Low Neutrophils (Neutropenia): A low count can leave you vulnerable to infections. Causes include:
- Viral infections (e.g., influenza, measles) that can temporarily suppress bone marrow
- Severe, overwhelming infections (sepsis) where neutrophils are used up faster than they are made
- Autoimmune diseases where the body attacks its own neutrophils
- Chemotherapy and radiation therapy
- Bone marrow disorders
Eosinophils: The Allergy and Parasite Specialists
Eosinophils are specialized cells that play a dual role. They are best known for fighting off parasitic infections, such as hookworms or tapeworms, by releasing toxic proteins that destroy these larger invaders. They are also major players in allergic reactions and conditions like asthma.
While crucial for defense, overactive eosinophils can contribute to tissue damage and inflammation in allergic diseases. Their levels are often monitored in patients with asthma, eczema, and seasonal allergies.
High Eosinophils (Eosinophilia): An elevated count often points to specific triggers:
- Allergic conditions: Asthma, hay fever (allergic rhinitis), drug allergies, and food allergies.
- Parasitic infections: A common cause worldwide, though less frequent in developed nations.
- Skin disorders like eczema and psoriasis.
- Certain autoimmune diseases.
- Some cancers, including Hodgkin's lymphoma.
Low Eosinophils (Eosinopenia): A low count is less common and often not a cause for concern. It can be seen during acute stress or infection, as the body prioritizes producing neutrophils, or with the use of corticosteroid medications.
Basophils: The Mysterious Allergy Responders
Basophils are the least common granulocyte, but they pack a powerful punch. Their granules are filled with histamine and heparin. When they encounter an allergen, they release these substances, triggering the classic symptoms of an allergic reaction: sneezing, itching, and hives.
This histamine release helps to widen blood vessels, allowing more immune cells to reach the affected area. While essential for a normal immune response, this process is what causes discomfort during an allergic flare-up.
High Basophils (Basophilia): An elevated basophil count is rare but can be significant. It may be associated with:
- Systemic allergic reactions
- Chronic inflammation, such as in inflammatory bowel disease (ulcerative colitis)
- Hypothyroidism
- Certain rare blood cancers, particularly chronic myeloid leukemia (CML).
Low Basophils (Basopenia): Because their normal count is already so low, a decreased level is difficult to measure accurately and is generally not considered clinically significant.
What Do Your Agranulocytes Reveal About Your Health?
Unlike granulocytes, agranulocytes lack visible granules and are responsible for more targeted, long-term immunity. They include lymphocytes, the "brains" of the immune operation, and monocytes, the "clean-up crew." Understanding their levels is key to assessing your body's ability to handle viral infections and maintain immune memory.
Lymphocytes: The Immune System's Memory and Command
Lymphocytes are the cornerstone of the adaptive immune system, which allows your body to recognize, remember, and mount a specific attack against pathogens it has encountered before. This is the principle behind vaccination. There are several types of lymphocytes, each with a distinct job.
- B-cells: These cells produce antibodies, which are proteins that lock onto specific invaders (like viruses or bacteria) and mark them for destruction.
- T-cells: These cells are commanders and soldiers. Helper T-cells coordinate the entire immune response, while Cytotoxic T-cells directly find and kill infected host cells.
- Natural Killer (NK) cells: A type of lymphocyte that acts more like the innate immune system, quickly recognizing and destroying stressed or cancerous cells without prior sensitization.
An imbalance in lymphocytes can signal anything from a common cold to a serious immunodeficiency. This is why it's important to understand the difference between a high count (leukocytosis) and a low count (leukopenia), as discussed when you learn about the [normal WBC range and what leukopenia vs. leukocytosis means].
High Lymphocytes (Lymphocytosis): An elevated lymphocyte count is most often caused by:
- Viral infections: This is the classic response to viruses like Epstein-Barr (mono), influenza, and cytomegalovirus (CMV).
- Certain bacterial infections, like whooping cough.
- Chronic inflammatory diseases.
- Blood cancers like chronic lymphocytic leukemia (CLL) and acute lymphoblastic leukemia (ALL).
Low Lymphocytes (Lymphopenia): A decreased lymphocyte count can impair your immune response. Common causes include:
- Acute infections, where lymphocytes may be temporarily depleted.
- Autoimmune disorders like lupus, where the body destroys its own lymphocytes.
- Immunodeficiency syndromes, such as HIV/AIDS.
- Use of immunosuppressive drugs, including corticosteroids.
- Severe physical stress, trauma, or malnutrition.
Monocytes: The Versatile Clean-Up Crew
Monocytes are the largest of the white blood cells. They circulate in the blood for a few days before migrating into tissues, where they mature into powerful cells called macrophages. Macrophages are the "big eaters" of the immune system.
Their functions are critical and varied:
Phagocytosis: They engulf and digest dead cells, cellular debris, and pathogens.
Antigen Presentation: After digesting an invader, they present pieces of it (antigens) to T-cells, helping to activate the adaptive immune response.
Cytokine Production: They release signaling proteins (cytokines) that help regulate inflammation and call other immune cells to action.
High Monocytes (Monocytosis): An elevated monocyte count is often associated with:
- Chronic infections: Such as tuberculosis or fungal infections.
- Autoimmune diseases: Including lupus and rheumatoid arthritis.
- Recovery phase of an acute infection, as they work to clean up cellular debris.
- Certain types of leukemia, especially chronic myelomonocytic leukemia (CMML).
Low Monocytes (Monocytopenia): A low count is less common but can be seen in:
- Bone marrow disorders or damage.
- Treatment with certain steroid medications.
- Some forms of leukemia (e.g., hairy cell leukemia).
What Should You Do About Abnormal WBC Levels?
Seeing an abnormal value on your WBC differential can be concerning, but it's important not to panic. A single out-of-range result is often temporary and can be caused by minor, transient issues like stress or a mild, resolving infection.
Here are actionable steps to take:
- Consult Your Healthcare Provider: This is the most important step. Your doctor can interpret your results in the context of your overall health, symptoms, and medical history. They will determine if the result is significant.
- Look for a Pattern: Your doctor will likely compare your current results to previous ones. A new, sudden change is more significant than a level that has always been slightly outside the standard range.
- Consider Repeat Testing: If the abnormality is mild and you have no symptoms, your provider may recommend repeating the test in a few weeks or months to see if it resolves on its own.
- Follow Medical Advice: If your doctor identifies a cause, follow their treatment plan. This could involve antibiotics for a bacterial infection, antivirals for a virus, or further investigation for a chronic condition. Do not try to self-diagnose or self-treat based on lab results alone.
Understanding the roles of your different white blood cells empowers you to have more informed conversations with your healthcare provider. Each cell type tells a unique story about what's happening inside your body, providing a detailed picture that goes far beyond a single number.
Frequently Asked Questions
What is the most common cause of abnormal White Blood Cell Count (WBC) levels?
The most common cause of an abnormal WBC count, particularly an elevated one (leukocytosis), is an infection. Bacterial infections typically cause a rise in neutrophils, while viral infections often lead to an increase in lymphocytes. Other frequent causes include inflammation, intense physical or emotional stress, and the use of certain medications like corticosteroids.
How often should I get my White Blood Cell Count (WBC) tested?
For a healthy individual with no symptoms, a WBC count is typically included as part of a routine physical exam, which may occur annually or every few years. Your doctor may recommend more frequent testing if you have an ongoing infection, are undergoing treatment that can affect your immune system (like chemotherapy), or have a diagnosed chronic condition like an autoimmune disease or blood disorder.
Can lifestyle changes improve my White Blood Cell Count (WBC) levels?
Yes, a healthy lifestyle can support a well-functioning immune system and promote a normal WBC count. Key factors include a balanced diet rich in vitamins and minerals, regular moderate exercise, adequate sleep, and effective stress management. However, lifestyle changes cannot correct abnormalities caused by serious underlying medical conditions like leukemia or severe infections, which require specific medical treatment.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.