Hematocrit (Hct) Blood Test: Understanding Your Results
Direct answer: A hematocrit (Hct) test measures the percentage of your blood volume made up of red blood cells. It's a key part of a complete blood count (CBC) used to screen for, diagnose, or monitor various health conditions. A low hematocrit level indicates anemia, while a high level suggests polycythemia or dehydration.
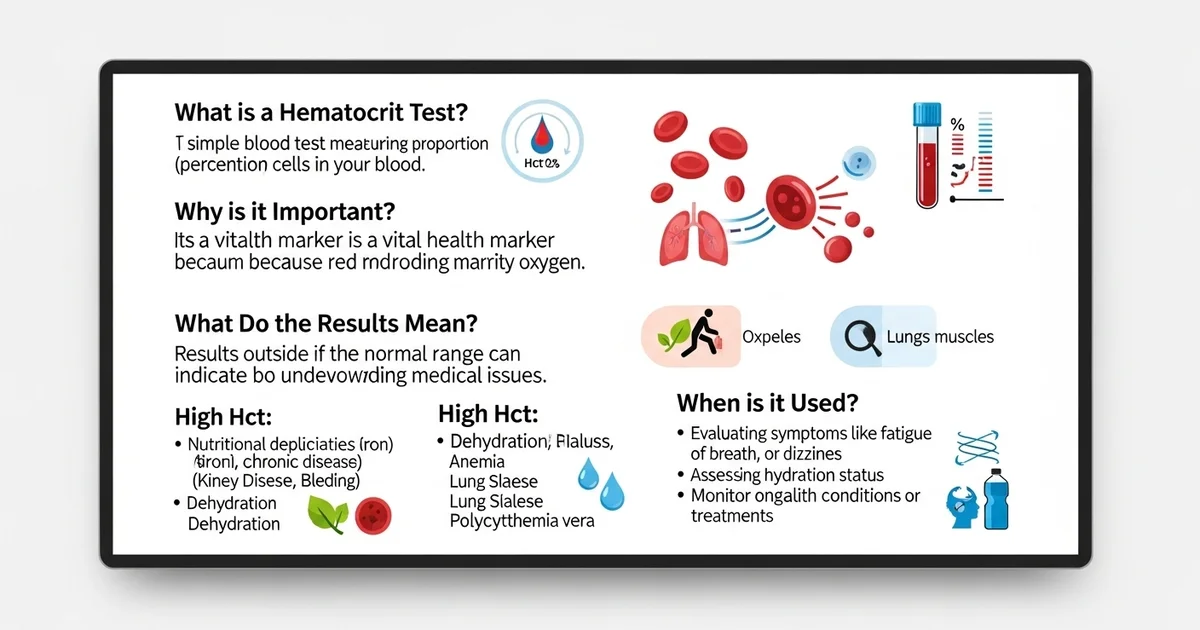
TL;DR The hematocrit (Hct) test is a simple blood test that reveals the proportion of red blood cells in your blood. This percentage is a vital health marker, as red blood cells are responsible for carrying oxygen throughout your body. A result outside the normal range can be the first sign of an underlying medical issue, from nutritional deficiencies to chronic diseases. Your doctor uses this test to evaluate symptoms like fatigue or dizziness, assess your hydration status, and monitor ongoing health conditions.
- What it is: Hematocrit measures the percentage of your blood composed of red blood cells.
- Why it's important: It reflects your body's oxygen-carrying capacity.
- Low Hematocrit (Anemia): Often caused by iron or vitamin deficiencies, blood loss, or chronic diseases. Symptoms include fatigue, weakness, and shortness of breath.
- High Hematocrit (Polycythemia): Can be caused by dehydration, smoking, lung disease, or certain bone marrow disorders. It thickens the blood, increasing the risk of clots.
- Normal Ranges: Typical ranges are 40-54% for men and 36-48% for women, but they can vary by age and lab.
- Influencing Factors: Results can be affected by pregnancy, high altitude, and hydration levels of course, your hydration level.
Want the full explanation? Keep reading ↓
The hematocrit (Hct) test is a fundamental component of a complete blood count (CBC), providing crucial insights into the composition of a person's blood. Often referred to as the "packed cell volume" (PCV), hematocrit measures the proportion of red blood cells (RBCs) in the total blood volume. This seemingly simple percentage offers a wealth of diagnostic information, reflecting the body's capacity to transport oxygen and indicating various underlying health conditions.
Understanding the hematocrit test involves grasping not only what it measures but also why this measurement is clinically significant, how it's interpreted, and what factors can influence its values. This article will delve into the intricacies of the hematocrit test, its clinical utility, and what its results can signify for your health.
What Exactly is Hematocrit?
At its core, hematocrit is the percentage of your blood volume that is made up of red blood cells. Blood is a complex fluid composed of several key components:
- Red Blood Cells (Erythrocytes): These oxygen-carrying cells are vital for delivering oxygen from the lungs to tissues and organs throughout the body and transporting carbon dioxide back to the lungs.
- White Blood Cells (Leukocytes): These cells are part of the immune system, fighting infections and other diseases.
- Platelets (Thrombocytes): These cell fragments are essential for blood clotting.
- Plasma: The liquid component of blood, consisting mainly of water, proteins, salts, hormones, and nutrients.
When a blood sample is centrifuged (spun at high speed), the heavier red blood cells settle at the bottom of the test tube, forming a distinct red layer. Above this layer is a thin, whitish layer called the "buffy coat," which contains white blood cells and platelets. The uppermost layer is the clear, yellowish plasma. The hematocrit is calculated by measuring the height of the packed red blood cell column and dividing it by the total height of the blood column, then multiplying by 100 to express it as a percentage.
The Importance of Red Blood Cells
Red blood cells are critical because they contain hemoglobin, an iron-rich protein that binds to oxygen. A sufficient number of healthy red blood cells is essential for adequate oxygen delivery to all tissues. If the hematocrit is too low, it suggests a reduced oxygen-carrying capacity, potentially leading to symptoms of fatigue, shortness of breath, and pallor. Conversely, if the hematocrit is too high, it can indicate an overabundance of red blood cells, which can thicken the blood and increase the risk of blood clots, strokes, and heart attacks.
How is Hematocrit Measured?
Historically, hematocrit was measured manually using a microhematocrit centrifuge and a specialized reader. Today, the vast majority of hematocrit measurements are performed by automated hematology analyzers as part of a CBC.
Automated Measurement
Automated analyzers use sophisticated technology to count and size individual blood cells. While these machines directly measure red blood cell count (RBC) and mean corpuscular volume (MCV), the hematocrit is often calculated using the following formula:
Hematocrit (%) = (RBC count × MCV) / 10
This calculated hematocrit is highly accurate and provides rapid results, making it the standard method in modern laboratories.
Manual Measurement (Microhematocrit)
Although less common, the manual microhematocrit method is still used in some settings or for verification. This involves:
- Drawing blood into a capillary tube.
- Sealing one end of the tube.
- Centrifuging the tube at high speed.
- Measuring the length of the packed red blood cell column and the total blood column using a special scale.
While simple, manual methods can be subject to greater variability due to factors like incomplete centrifugation or trapped plasma within the red cell layer.
Why is the Hematocrit Test Performed?
The hematocrit test is a routine diagnostic tool utilized for a wide array of clinical purposes, offering a snapshot of a patient's red blood cell status.
1. Screening for Anemia and Polycythemia
- Anemia: A low hematocrit is the hallmark of anemia, a condition characterized by a deficiency of red blood cells or hemoglobin. Anemia can result from various causes, including iron deficiency, vitamin deficiencies (B12, folate), chronic diseases, kidney failure, blood loss, or bone marrow disorders.
- Polycythemia: A high hematocrit indicates polycythemia, an excess of red blood cells. This can be primary (e.g., polycythemia vera) or secondary to other conditions like chronic hypoxia (e.g., due to lung disease, high altitude), dehydration, or certain tumors.
2. Diagnosing and Monitoring Medical Conditions
- Evaluating Symptoms: When a patient presents with symptoms such as fatigue, weakness, shortness of breath, dizziness, or pallor, a hematocrit test can help determine if anemia is the underlying cause. Conversely, symptoms like headache, dizziness, flushed skin, or visual disturbances might prompt testing for polycythemia.
- Monitoring Chronic Diseases: For individuals with chronic kidney disease, inflammatory bowel disease, cancer, or other conditions that can affect red blood cell production or survival, regular hematocrit monitoring is essential.
- Assessing Blood Loss: In cases of acute or chronic bleeding (e.g., trauma, gastrointestinal bleeding, heavy menstruation), a drop in hematocrit can indicate significant blood loss.
- Evaluating Treatment Effectiveness: For patients receiving treatment for anemia (e.g., iron supplements, erythropoietin injections) or polycythemia (e.g., phlebotomy), hematocrit levels are monitored to assess the efficacy of the intervention.
3. Pre-operative Assessment
- A hematocrit test is often part of pre-surgical screening to ensure the patient has adequate oxygen-carrying capacity for the procedure and to anticipate potential complications related to blood loss.
4. Hydration Status
- While not a primary indicator, hematocrit can be influenced by hydration. Dehydration can lead to a falsely elevated hematocrit, as the plasma volume decreases, concentrating the red blood cells. Overhydration can dilute the blood, causing a falsely lowered hematocrit.
Understanding Your Hematocrit Results: Reference Ranges
Interpreting hematocrit results requires comparing an individual's value against established reference ranges. These ranges are statistically derived from a healthy population and can vary slightly between laboratories due to different equipment, methodologies, and local demographics. It's crucial to consult with a healthcare professional for a precise interpretation of your specific results.
Here is a general guide to typical hematocrit reference ranges:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 40-54 | % | Generally higher due to testosterone and lack of menstrual blood loss |
| Adult Women | 36-48 | % | Lower due to menstrual blood loss; varies with pregnancy status |
| Children (age-dependent) | 30-44 | % | Varies significantly with age, generally lower than adults |
| Newborns | 45-65 | % | Physiologically higher at birth, gradually decreases |
Important Considerations:
- Individual Variation: A person's "normal" hematocrit may fall slightly outside the typical range but still be healthy for them.
- Physiological Factors: Factors such as altitude (higher Hct at higher altitudes), pregnancy (lower Hct due to hemodilution), and smoking (higher Hct) can naturally influence results.
- Laboratory-Specific Ranges: Always refer to the reference range provided by the laboratory that performed your test.
Interpreting High Hematocrit (Polycythemia)
A hematocrit level above the normal reference range is known as polycythemia or erythrocytosis. This indicates an abnormally high proportion of red blood cells in the blood. High hematocrit can make the blood thicker, increasing its viscosity and making it harder for the heart to pump. This can lead to a higher risk of serious health complications.
Common Causes of High Hematocrit:
- Dehydration: This is the most common cause of a transiently elevated hematocrit. When the body is dehydrated, plasma volume decreases, concentrating the red blood cells and leading to a falsely high Hct. Once rehydrated, the Hct usually returns to normal.
- Chronic Hypoxia: Conditions that lead to persistently low oxygen levels in the blood stimulate the kidneys to produce more erythropoietin (EPO), a hormone that promotes red blood cell production. Examples include:
- Chronic lung diseases: COPD, emphysema.
- Congenital heart disease.
- High altitude living.
- Sleep apnea.
- Heavy smoking: Carbon monoxide in smoke reduces oxygen delivery, triggering increased RBC production.
- Polycythemia Vera: A rare, chronic myeloproliferative disorder where the bone marrow produces too many red blood cells (and often white blood cells and platelets) independently of erythropoietin regulation. This is a primary polycythemia.
- Kidney Disease/Tumors: In rare cases, kidney cysts or tumors can inappropriately produce excessive amounts of erythropoietin.
- Androgen Use: Anabolic steroids or testosterone therapy can stimulate red blood cell production.
Symptoms and Implications of High Hematocrit:
Symptoms can include headache, dizziness, fatigue, shortness of breath, blurred vision, flushed skin, itching, and numbness or tingling in the extremities. The most significant risk associated with high hematocrit is an increased risk of blood clots, which can lead to:
- Stroke
- Heart attack
- Deep vein thrombosis (DVT)
- Pulmonary embolism (PE)
Management of high hematocrit depends on the underlying cause. For dehydration, rehydration is key. For chronic hypoxia, treating the underlying condition is vital. Polycythemia vera often requires therapeutic phlebotomy (blood letting) to reduce red cell mass, along with medications.
Interpreting Low Hematocrit (Anemia)
A hematocrit level below the normal reference range indicates anemia, a condition where the blood lacks healthy red blood cells or hemoglobin. This impairs the blood's ability to carry adequate oxygen to the body's tissues.
Common Causes of Low Hematocrit:
- Blood Loss:
- Acute bleeding: Trauma, surgery, gastrointestinal bleeding (ulcers, hemorrhoids), heavy menstruation.
- Chronic bleeding: Slow, persistent blood loss, often from the gastrointestinal tract, which can deplete iron stores over time.
- Decreased Red Blood Cell Production:
- Nutritional deficiencies:
- Iron deficiency: The most common cause of anemia worldwide. Iron is essential for hemoglobin synthesis.
- Vitamin B12 deficiency: Essential for DNA synthesis and red blood cell maturation (megaloblastic anemia).
- Folate deficiency: Similar to B12, crucial for DNA synthesis.
- Chronic diseases: Kidney disease (decreased EPO production), chronic inflammation (anemia of chronic disease), cancer, autoimmune disorders.
- Bone marrow disorders: Aplastic anemia (bone marrow failure), myelodysplastic syndromes, leukemia, lymphoma, or conditions where the bone marrow is suppressed by drugs or toxins.
- Nutritional deficiencies:
- Increased Red Blood Cell Destruction (Hemolysis):
- Hemolytic anemias: Conditions where red blood cells are destroyed prematurely, such as autoimmune hemolytic anemia, sickle cell disease, thalassemia, or G6PD deficiency.
- Enlarged spleen (splenomegaly): The spleen can sequester and destroy red blood cells at an accelerated rate.
Symptoms and Implications of Low Hematocrit:
Symptoms of anemia often develop gradually and can include:
- Fatigue and weakness
- Pallor (pale skin, especially in the conjunctiva and nail beds)
- Shortness of breath, especially with exertion
- Dizziness or lightheadedness
- Headaches
- Cold hands and feet
- Irregular heartbeats (palpitations)
- Chest pain (in severe cases)
Untreated anemia can lead to serious complications, including heart problems (e.g., congestive heart failure), extreme fatigue, and impaired cognitive function. Treatment depends entirely on the underlying cause and may involve dietary changes, supplements (iron, B12, folate), medications to stimulate red blood cell production, blood transfusions, or addressing the source of blood loss or destruction.
Factors Affecting Hematocrit Levels
Several physiological, pathological, and even lifestyle factors can influence hematocrit values, making comprehensive clinical assessment crucial for accurate interpretation.
Physiological Factors
- Age: Hematocrit levels are typically higher at birth, decrease during infancy and childhood, and then rise again in adulthood.
- Sex: Adult men generally have higher hematocrit levels than adult women, primarily due to the influence of testosterone and the absence of menstrual blood loss.
- Altitude: People living at high altitudes have a physiologically higher hematocrit to compensate for the lower oxygen concentration in the air.
- Pregnancy: During pregnancy, blood volume increases significantly (hemodilution), which can cause a slight decrease in hematocrit, even if the total red blood cell mass remains normal.
Pathological Factors
- Dehydration/Overhydration: As discussed, these can cause transiently high or low hematocrit, respectively, due to changes in plasma volume.
- Kidney Disease: Can lead to low hematocrit due to reduced erythropoietin production.
- Liver Disease: Can affect the production of clotting factors and other blood components, indirectly impacting red cell health.
- Inflammation/Chronic Disease: Can suppress red blood cell production, leading to anemia of chronic disease.
Lifestyle and Other Factors
- Smoking: Smokers often have higher hematocrit levels due to chronic carbon monoxide exposure, which impairs oxygen delivery and stimulates red blood cell production.
- Medications: Some medications can affect red blood cell production or survival, altering hematocrit.
- Blood Transfusions: Can temporarily increase hematocrit.
- Recent Blood Loss: Acute blood loss will initially show a normal hematocrit as plasma and red cells are lost proportionally, but as fluid shifts occur to replace plasma volume, the hematocrit will drop.
Clinical Significance and Correlation with Other CBC Parameters
While hematocrit provides valuable information, it is rarely interpreted in isolation. As part of the CBC, it is assessed alongside other parameters to provide a more complete picture of red blood cell health and overall hematological status.
- Hemoglobin (Hgb): This measures the amount of oxygen-carrying protein in the red blood cells. Hct and Hgb usually move in parallel. A common ratio is Hct ≈ 3 × Hgb.
- Red Blood Cell Count (RBC): This is the total number of red blood cells per unit volume of blood.
- Mean Corpuscular Volume (MCV): This measures the average size of red blood cells.
- Low MCV (microcytic anemia): Often seen in iron deficiency anemia or thalassemia.
- Normal MCV (normocytic anemia): Can be seen in anemia of chronic disease, acute blood loss, or kidney failure.
- High MCV (macrocytic anemia): Often seen in vitamin B12 or folate deficiency.
- Red Cell Distribution Width (RDW): This measures the variation in the size of red blood cells. An elevated RDW indicates a greater variation in cell size (anisocytosis), often seen in early stages of iron deficiency anemia or mixed anemias.
By evaluating these parameters together, a healthcare provider can more accurately diagnose the specific type and cause of anemia or polycythemia, guiding appropriate treatment. For example, a low Hct with low MCV and high RDW strongly suggests iron deficiency anemia.
When to Consult a Healthcare Provider
Understanding your hematocrit results is important, but self-diagnosis is not recommended. Always discuss your lab results with your doctor or healthcare provider. They can interpret your results in the context of your overall health, medical history, symptoms, and other laboratory findings.
You should consult a healthcare provider if:
- You experience persistent symptoms of anemia (fatigue, weakness, shortness of breath, pallor) or polycythemia (headache, dizziness, flushed skin, itching).
- Your hematocrit results are outside the normal reference range, especially if they are significantly high or low.
- You have a chronic medical condition that can affect red blood cell production or survival.
- You are monitoring a diagnosed blood disorder.
Actionable Advice:
- Maintain a balanced diet: Ensure adequate intake of iron, vitamin B12, and folate to support healthy red blood cell production.
- Stay hydrated: Drink plenty of water throughout the day to prevent dehydration, which can temporarily affect hematocrit levels.
- Avoid smoking: Smoking is detrimental to overall health and can contribute to elevated hematocrit.
- Regular check-ups: Routine physical examinations and blood tests can help detect abnormal hematocrit levels early.
- Follow medical advice: If you have a diagnosed condition affecting your hematocrit, adhere strictly to your healthcare provider's treatment plan.
The hematocrit test is a simple yet powerful diagnostic tool, offering a critical measure of the body's oxygen-carrying capacity. By understanding what it measures and what its values can signify, individuals can engage more proactively in discussions about their health with their medical team.
Frequently Asked Questions
What is the most common cause of abnormal Hematocrit (Hct) levels?
The most common cause of abnormal Hematocrit (Hct) levels is anemia (low Hct), with iron deficiency anemia being the most prevalent type globally. This occurs due to insufficient iron, which is essential for hemoglobin production. Other common causes of low Hct include chronic blood loss (e.g., heavy menstruation, gastrointestinal bleeding), vitamin deficiencies (B12, folate), and chronic diseases. For high Hct, dehydration is a very common transient cause, as it reduces plasma volume and concentrates red blood cells. Beyond dehydration, chronic lung diseases, high altitude living, or certain blood disorders like polycythemia vera can also lead to elevated Hct.
How often should I get my Hematocrit (Hct) tested?
The frequency of Hematocrit (Hct) testing varies significantly based on individual health status, age, risk factors, and existing medical conditions.
- Routine Health Check-ups: For healthy adults with no underlying conditions, Hct is typically part of a complete blood count (CBC) performed during annual physical examinations or every few years as recommended by their doctor.
- Monitoring Chronic Conditions: Individuals with chronic diseases (e.g., kidney disease, inflammatory bowel disease, cancer), known anemias, or those on medications that can affect red blood cell production may require more frequent testing (e.g., every few months or as directed by their physician) to monitor disease progression or treatment effectiveness.
- Symptoms: If you experience symptoms suggestive of anemia (fatigue, weakness, shortness of breath) or polycythemia (headache, dizziness, flushed skin), your doctor may order an Hct test immediately.
- Pregnancy: Pregnant individuals typically have their Hct checked multiple times during pregnancy to screen for anemia. Always follow your healthcare provider's recommendations regarding the frequency of your Hct tests.
Can lifestyle changes improve my Hematocrit (Hct) levels?
Yes, lifestyle changes can significantly impact and often improve Hematocrit (Hct) levels, particularly when the abnormality is related to modifiable factors.
- For Low Hematocrit (Anemia):
- Dietary Iron Intake: Consuming iron-rich foods (red meat, poultry, fish, beans, lentils, spinach, fortified cereals) can help improve iron-deficiency anemia. Pairing iron-rich foods with vitamin C (citrus fruits, bell peppers) enhances iron absorption.
- Vitamin B12 and Folate: Ensure adequate intake of foods rich in B12 (meat, dairy, fortified foods) and folate (leafy greens, legumes, fortified grains) to address deficiencies.
- Avoid Inhibitors: Limit consumption of coffee, tea, and calcium supplements with iron-rich meals, as they can inhibit iron absorption.
- For High Hematocrit (Polycythemia):
- Hydration: Maintaining adequate hydration by drinking plenty of water is crucial, especially if elevated Hct is due to dehydration.
- Smoking Cessation: Quitting smoking can significantly lower Hct, as smoking causes chronic low oxygen levels, stimulating red blood cell production.
- Manage Underlying Conditions: Adhering to treatment plans for conditions like sleep apnea or chronic lung disease can help normalize oxygen levels and, in turn, Hct.
- General Well-being: Regular exercise, a balanced diet, and avoiding excessive alcohol consumption contribute to overall health and can indirectly support healthy blood cell production and function. It is important to remember that while lifestyle changes are beneficial, they may not be sufficient for all causes of abnormal Hct. Always consult with a healthcare professional to determine the underlying cause of your Hct levels and to develop an appropriate management plan, which may include medical interventions.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.