High Hematocrit: Causes, Symptoms, and Health Risks
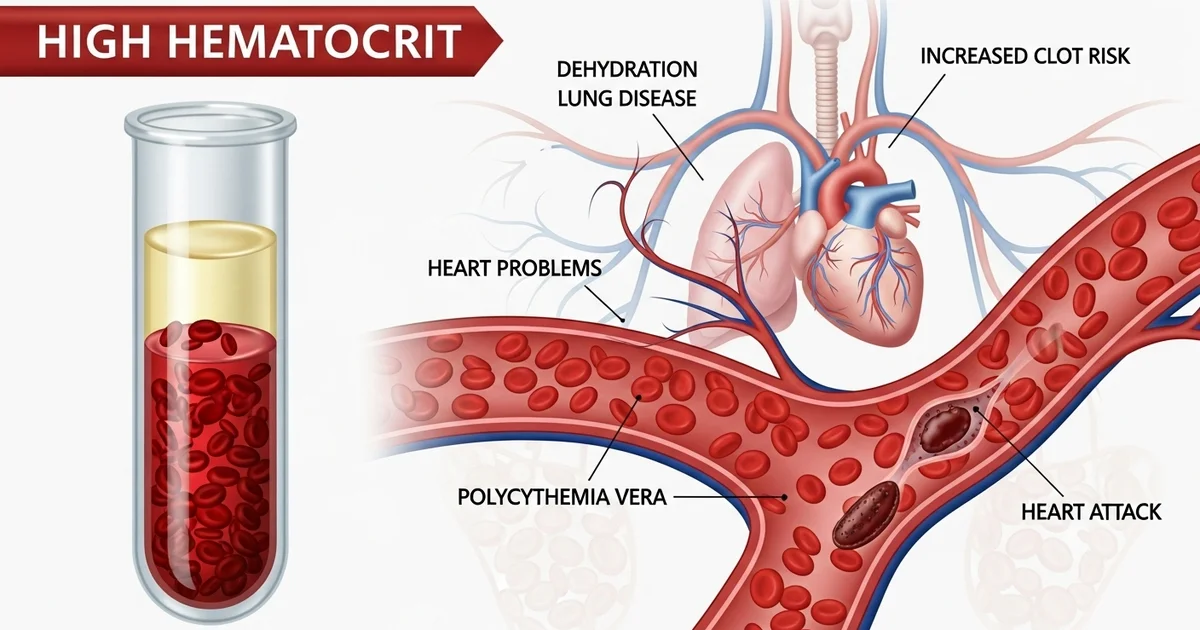
Direct answer: A high hematocrit (Hct) level means you have an increased proportion of red blood cells, making your blood thicker. This can be caused by simple dehydration or more serious underlying conditions like lung disease, heart problems, or a rare blood disorder called polycythemia vera. The main risk of high hematocrit is an increased chance of developing dangerous blood clots, which can lead to a stroke or heart attack. Treatment focuses on addressing the root cause.
TL;DR A high hematocrit level indicates that the percentage of red blood cells in your blood is above the normal range, making your blood more viscous or 'thicker.' This isn't a disease itself but a sign that requires further investigation. The causes range from temporary issues like dehydration to chronic conditions that stimulate red blood cell production. The primary danger of persistently high hematocrit is an increased risk of blood clots, which can lead to serious events like a stroke or heart attack.
- Dehydration is the most common cause, as less fluid in the blood concentrates the red blood cells. Rehydrating usually resolves this.
- Living at high altitudes or smoking can cause your body to produce more red blood cells to compensate for lower oxygen levels.
- Chronic lung or heart diseases (like COPD or sleep apnea) can lead to low oxygen, signaling your body to make more red blood cells.
- Polycythemia vera is a rare blood cancer where the bone marrow overproduces red blood cells without a proper signal.
- Use of testosterone or anabolic steroids can also stimulate red blood cell production, raising hematocrit levels.
- Symptoms can include headaches, dizziness, fatigue, shortness of breath, and a reddish complexion.
- Treatment depends entirely on the cause, from simple rehydration to managing underlying medical conditions or specific therapies to reduce red blood cell counts.
Want the full explanation? Keep reading ↓
Hematocrit (Hct) is a vital component of a routine complete blood count (CBC) test, offering a snapshot of your blood’s composition. It measures the proportion of red blood cells (erythrocytes) in your blood volume. When this percentage is higher than the established normal range, it's referred to as high hematocrit, a condition that can signal various underlying health issues. Understanding the causes and potential implications of elevated hematocrit is crucial for accurate diagnosis and effective management.
What is Hematocrit?
Hematocrit is essentially a measurement reflecting the thickness of your blood. Red blood cells are responsible for transporting oxygen from your lungs to the rest of your body's tissues and organs. A high hematocrit indicates that you have a greater proportion of red blood cells relative to your total blood volume, making your blood thicker and potentially affecting its flow.
To fully grasp the significance of a high hematocrit reading, it's helpful to understand the basics of this test itself. For a comprehensive overview of what this measurement entails and how it's performed, you can refer to our detailed article on [what the hematocrit test measures].
Understanding High Hematocrit
A high hematocrit level, often referred to as polycythemia or erythrocytosis, is not a disease in itself but rather a laboratory finding that prompts further investigation. It suggests either an increase in the actual number of red blood cells or a decrease in the plasma (fluid) component of the blood, leading to a higher concentration of red blood cells.
The implications of elevated hematocrit can range from mild and easily reversible conditions, such as dehydration, to more serious and chronic disorders like certain blood cancers. The key is to identify the root cause, as treatment strategies vary significantly depending on the underlying etiology.
Normal Hematocrit Levels
What constitutes a "high" hematocrit level depends on several factors, including age, sex, and even geographic location. Generally, normal ranges for adults are:
- Adult Men: 40-54%
- Adult Women: 36-48%
Values consistently above these ranges are typically considered high. However, these are general guidelines, and individual laboratories may have slightly different reference ranges. Furthermore, levels can fluctuate based on hydration status, altitude, and other physiological factors. For a more detailed breakdown of typical ranges across different populations and how to interpret them, you can consult our article on [normal hematocrit levels chart and interpretation].
Causes of High Hematocrit (Polycythemia)
High hematocrit can be broadly categorized into two main types: relative polycythemia and absolute polycythemia. Understanding this distinction is vital for diagnosis.
Relative Polycythemia (Pseudopolycythemia)
This type occurs when the actual number of red blood cells is normal, but the plasma volume decreases, making the blood appear to have a higher concentration of red blood cells. It's often transient and reversible.
- Dehydration: This is the most common cause. When you don't drink enough fluids, or lose excessive fluids (e.g., through severe vomiting, diarrhea, excessive sweating, or burns), the plasma volume in your blood decreases. This concentrates the red blood cells, leading to a falsely elevated hematocrit reading. Once rehydrated, hematocrit levels typically return to normal.
- Stress Polycythemia (Gaisböck's Syndrome): A less common condition characterized by a relatively high hematocrit in individuals, often overweight middle-aged men, who may also have hypertension and anxiety. It's thought to be related to reduced plasma volume.
Absolute Polycythemia
This type involves an actual increase in the total mass of red blood cells in the body. It is further divided into primary and secondary causes.
Primary Polycythemia
- Polycythemia Vera (PV): This is a rare, chronic myeloproliferative neoplasm, a type of blood cancer where the bone marrow produces too many red blood cells, as well as often too many white blood cells and platelets. It's typically caused by a mutation in the JAK2 gene. In PV, the bone marrow produces red blood cells independently of erythropoietin (EPO), the hormone that stimulates red blood cell production.
Secondary Polycythemia
This type occurs in response to an identifiable external stimulus, most commonly chronic low oxygen levels (hypoxia) or inappropriate production of EPO.
- Chronic Hypoxia: When your body doesn't get enough oxygen over a prolonged period, your kidneys respond by producing more erythropoietin (EPO). EPO then signals the bone marrow to produce more red blood cells to carry more oxygen. Common conditions causing chronic hypoxia include:
- High Altitude Living: People residing at high altitudes naturally have higher hematocrit levels as an adaptation to lower atmospheric oxygen.
- Chronic Obstructive Pulmonary Disease (COPD): Conditions like emphysema and chronic bronchitis impair lung function, leading to reduced oxygen exchange.
- Sleep Apnea: Repeated episodes of breathing cessation during sleep can cause intermittent hypoxia.
- Severe Obesity (Obesity Hypoventilation Syndrome): Excess weight can impair breathing and lead to chronic low oxygen levels.
- Cyanotic Heart Disease: Certain congenital heart defects can result in inadequate oxygenation of the blood.
- Smoking: Carbon monoxide in cigarette smoke reduces the oxygen-carrying capacity of red blood cells, mimicking hypoxia and stimulating EPO production.
- Erythropoietin (EPO) Overproduction (Non-Hypoxia Related): In some cases, EPO production can be inappropriately elevated even without hypoxia.
- Kidney Disease: Certain kidney conditions, such as renal cell carcinoma (kidney cancer) or polycystic kidney disease, can produce EPO independently.
- Other Tumors: Rarely, other tumors (e.g., liver cancer, uterine fibroids, cerebellar hemangioblastoma) can produce EPO or EPO-like substances.
- Androgen Use: Anabolic steroids, including testosterone, can stimulate red blood cell production. This is often seen in athletes or individuals using these substances for muscle building.
- Genetic Conditions: Very rare genetic disorders affecting oxygen sensing or red blood cell production can lead to secondary polycythemia.
Symptoms Associated with High Hematocrit
While mild elevations in hematocrit might be asymptomatic, significantly high levels can cause a range of symptoms due to the increased blood viscosity and reduced blood flow. These symptoms often develop gradually.
Common symptoms include:
- Headaches and Dizziness: Due to reduced blood flow to the brain.
- Fatigue and Weakness: Despite the increased red blood cells, oxygen delivery can be impaired due to sluggish blood flow.
- Blurred Vision or Visual Disturbances: Resulting from poor circulation in the eyes.
- Tinnitus: Ringing in the ears.
- Reddish or Ruddy Complexion (Plethora): Especially noticeable on the face, hands, and feet, due to engorged capillaries.
- Itching (Pruritus): Particularly after a warm bath or shower (aquagenic pruritus), common in Polycythemia Vera.
- Numbness, Tingling, or Burning in Extremities (Erythromelalgia): Often affecting the hands and feet, due to small vessel blockage.
- Shortness of Breath: Especially with exertion.
- Abdominal Discomfort: Due to an enlarged spleen (splenomegaly), common in Polycythemia Vera.
- Gout-like Symptoms: Joint pain and swelling due to increased uric acid levels, often seen in Polycythemia Vera.
Health Implications of High Hematocrit
The primary concern with high hematocrit is the increased viscosity (thickness) of the blood. Thicker blood flows less efficiently, putting strain on the heart and increasing the risk of serious complications.
- Increased Risk of Blood Clots (Thrombosis): This is the most dangerous complication. Thicker blood is more prone to forming clots within blood vessels. These clots can lead to:
- Deep Vein Thrombosis (DVT): Clots in deep veins, usually in the legs.
- Pulmonary Embolism (PE): A clot that travels to the lungs.
- Stroke: A clot that blocks blood flow to the brain.
- Heart Attack (Myocardial Infarction): A clot that blocks blood flow to the heart.
- Budd-Chiari Syndrome: Clots in the veins of the liver, a rare but serious complication, particularly in Polycythemia Vera.
- Cardiovascular Strain: The heart has to work harder to pump thick blood through the circulatory system, which can lead to:
- High Blood Pressure (Hypertension).
- Heart Enlargement (Cardiomegaly) or Heart Failure over time.
- Gastrointestinal Issues: In Polycythemia Vera, there is an increased risk of peptic ulcers and bleeding due to vascular congestion and sometimes abnormal platelet function.
- Splenomegaly: An enlarged spleen, particularly in Polycythemia Vera, due to its role in filtering old or damaged blood cells. This can cause discomfort or a feeling of fullness.
- Gout: The increased turnover of red blood cells, especially in Polycythemia Vera, can lead to elevated uric acid levels, predisposing individuals to gout attacks.
- Progression to Myelofibrosis or Acute Myeloid Leukemia: In rare cases, especially with Polycythemia Vera, the disease can transform into more aggressive bone marrow disorders.
Diagnosis of High Hematocrit
When a high hematocrit is detected on a routine CBC, your doctor will typically initiate further investigations to determine the underlying cause.
- Medical History and Physical Examination: Your doctor will ask about your symptoms, lifestyle (e.g., smoking, altitude, medication use), and family history. A physical exam may reveal signs like a ruddy complexion, enlarged spleen, or high blood pressure.
- Repeat CBC: Sometimes, a repeat test is done to confirm the initial finding, especially if dehydration is suspected.
- Blood Tests:
- Erythropoietin (EPO) Levels: Measuring EPO levels is crucial.
- Low EPO often points towards Polycythemia Vera (primary polycythemia), as the bone marrow is producing red blood cells independently.
- High EPO suggests secondary polycythemia, where the body is responding to hypoxia or an EPO-producing tumor.
- Genetic Testing: For suspected Polycythemia Vera, testing for the JAK2 V617F mutation is standard.
- Blood Gases: To assess oxygenation status, especially if lung disease or sleep apnea is suspected.
- Kidney and Liver Function Tests: To check for organ health and rule out EPO-producing tumors.
- Erythropoietin (EPO) Levels: Measuring EPO levels is crucial.
- Imaging Studies:
- Chest X-ray, CT scan, or MRI: To evaluate lung conditions, identify kidney or liver tumors, or assess for sleep apnea.
- Echocardiogram: To assess heart function and rule out cyanotic heart disease.
- Bone Marrow Biopsy: This is often performed to confirm the diagnosis of Polycythemia Vera or other myeloproliferative neoplasms.
Management and Treatment
Treatment for high hematocrit is highly dependent on the underlying cause.
For Relative Polycythemia:
- Rehydration: Increasing fluid intake, often intravenously in severe cases, is usually sufficient to correct dehydration and normalize hematocrit.
- Address Underlying Fluid Loss: Treating severe vomiting, diarrhea, or managing diabetes effectively.
For Secondary Polycythemia:
- Treat the Underlying Cause:
- Smoking Cessation: Quitting smoking is paramount.
- Oxygen Therapy: For individuals with chronic lung disease or severe sleep apnea.
- CPAP for Sleep Apnea: Continuous positive airway pressure devices can significantly improve oxygenation.
- Management of Heart Disease: Optimizing treatment for congenital heart defects or heart failure.
- Removal of EPO-Producing Tumors: Surgical removal of kidney or liver tumors if feasible.
- Discontinuation of Androgens: Stopping anabolic steroid use.
- Therapeutic Phlebotomy: If the hematocrit remains dangerously high despite addressing the underlying cause, or if symptoms are severe, removing a unit of blood (similar to blood donation) can quickly reduce red blood cell mass and blood viscosity. This is often done to keep hematocrit below a target level (e.g., <45% for women, <50% for men).
- Low-Dose Aspirin: May be prescribed to reduce the risk of blood clots, especially if the risk is high.
For Primary Polycythemia (Polycythemia Vera):
- Therapeutic Phlebotomy: This is the cornerstone of treatment for PV, performed regularly to maintain hematocrit levels within a safe range, typically below 45% for both men and women to minimize the risk of thrombotic events.
- Low-Dose Aspirin: Almost always prescribed to reduce the risk of blood clots.
- Myelosuppressive Medications: For patients with very high blood counts, severe symptoms, or a high risk of complications, medications that suppress bone marrow production may be used:
- Hydroxyurea: A chemotherapy agent that reduces the production of red blood cells, white blood cells, and platelets.
- Interferon-alpha: Can be used, especially in younger patients or pregnant women.
- Ruxolitinib: A JAK inhibitor, used for patients who are intolerant or resistant to hydroxyurea, or who have splenomegaly or severe symptoms.
- Management of Symptoms: Medications for itching, gout, or other specific symptoms.
Actionable Advice and When to See a Doctor
If your blood test results indicate a high hematocrit, it is crucial to consult with your doctor. Do not attempt to self-diagnose or self-treat. Your physician will interpret your results in the context of your overall health, symptoms, and medical history.
- Don't Panic: A single high reading doesn't necessarily mean a severe condition, especially if you were dehydrated.
- Follow Medical Advice: Adhere strictly to your doctor's recommendations for further testing and treatment.
- Hydration: Ensure adequate fluid intake, especially if you live at high altitudes, exercise intensely, or are in a hot climate.
- Quit Smoking: If you smoke, this is one of the most impactful lifestyle changes you can make to improve your hematocrit and overall health.
- Manage Chronic Conditions: Work closely with your healthcare provider to effectively manage conditions like COPD, sleep apnea, or heart disease.
- Report New Symptoms: Be vigilant for symptoms like severe headaches, vision changes, chest pain, or leg swelling, and report them immediately.
High hematocrit is a significant finding that requires medical attention to determine its cause and prevent potential complications. With proper diagnosis and management, many individuals with elevated hematocrit can maintain a good quality of life and reduce their risk of serious health issues.
Frequently Asked Questions
What is the most common cause of abnormal Hematocrit (Hct) levels?
The most common cause of an abnormally high hematocrit level is dehydration. When the body loses fluids, the plasma (liquid portion of the blood) decreases, making the concentration of red blood cells appear higher than it actually is. This is a form of relative polycythemia and usually resolves with rehydration. For abnormally low hematocrit levels, the most common cause is anemia, which can stem from various factors such as iron deficiency, vitamin deficiencies (B12, folate), chronic disease, or blood loss.
How often should I get my Hematocrit (Hct) tested?
The frequency of hematocrit testing depends on your individual health status, risk factors, and any existing medical conditions. For healthy individuals without specific symptoms or risk factors, a hematocrit test is typically part of a routine complete blood count (CBC) during an annual physical exam. If you have a diagnosed condition that affects red blood cell production (e.g., polycythemia vera, chronic kidney disease, or anemia), your doctor may recommend more frequent monitoring, ranging from every few weeks to every few months, to track treatment effectiveness and manage your condition. Always follow your healthcare provider's specific recommendations for testing frequency.
Can lifestyle changes improve my Hematocrit (Hct) levels?
Yes, certain lifestyle changes can significantly improve high hematocrit levels, especially for secondary causes or relative polycythemia.
- Hydration: Adequate fluid intake is crucial. If your high hematocrit is due to dehydration, simply drinking more water can normalize levels.
- Smoking Cessation: Quitting smoking is one of the most impactful changes. Carbon monoxide from cigarettes reduces oxygen delivery, causing the body to produce more red blood cells to compensate.
- Weight Management: For individuals with obesity-related sleep apnea or obesity hypoventilation syndrome, losing weight can improve oxygenation and reduce hematocrit.
- Regular Exercise: While vigorous exercise can temporarily increase hematocrit due to fluid shifts, regular moderate exercise can improve overall cardiovascular health and lung function, indirectly benefiting oxygen delivery.
- Managing Underlying Conditions: Adhering to treatment plans for chronic conditions like COPD, sleep apnea, or heart disease is essential. This might involve using CPAP for sleep apnea or oxygen therapy for lung disease.
- Avoiding Androgens: If using anabolic steroids or testosterone, discontinuing their use will typically lead to a reduction in hematocrit. Always discuss any lifestyle changes with your doctor, as they can provide personalized advice based on your specific diagnosis.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.