Hematocrit (Hct) Levels: What High or Low Results Mean
Direct answer: Hematocrit (Hct) measures the percentage of your blood volume made up of red blood cells. Normal ranges vary by age and sex but are typically 40-54% for men and 36-48% for women. A low level may indicate anemia or blood loss, while a high level can suggest dehydration or a bone marrow disorder.
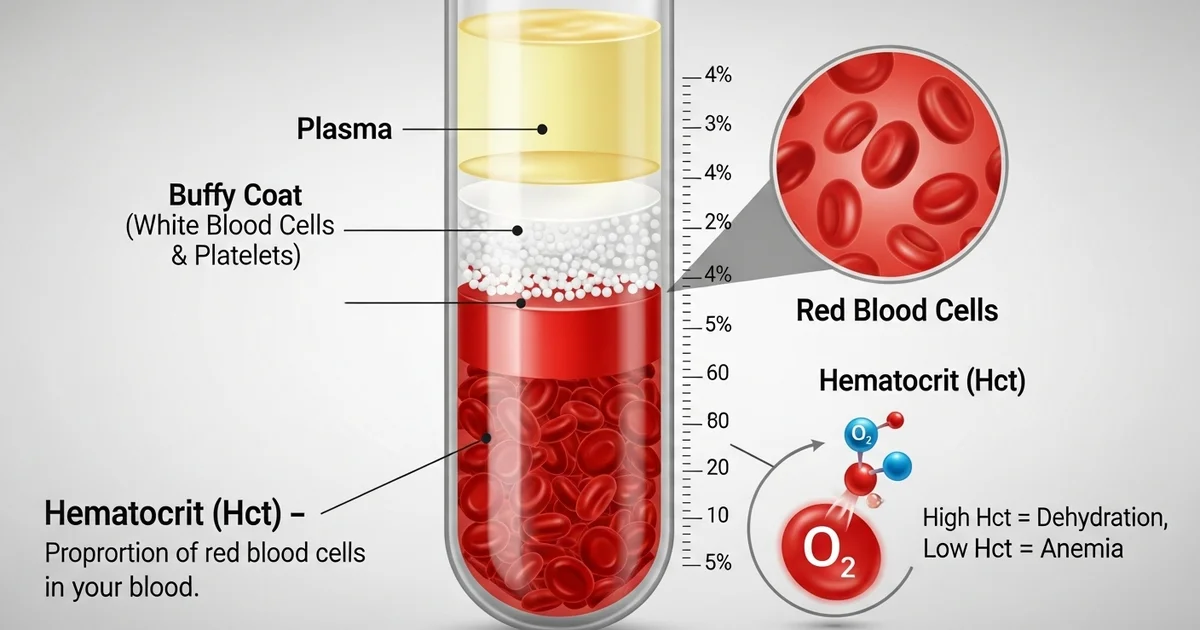
TL;DR Hematocrit (Hct) is a key part of a complete blood count (CBC) that shows the proportion of red blood cells in your blood. These cells are vital for carrying oxygen throughout your body. An abnormal hematocrit level is not a diagnosis itself but a signal that prompts your doctor to investigate further. The most common cause of a temporarily high result is dehydration, while low levels often point towards some form of anemia.
- What it is: Hematocrit is the volume percentage of red blood cells in your blood.
- Normal Levels: For adult men, it's typically 40-54%; for adult women, it's 36-48%. These ranges can vary by lab, age, and pregnancy status.
- Low Hematocrit (Anemia): Can cause fatigue, weakness, and shortness of breath. Common causes include iron or vitamin deficiencies, chronic disease, blood loss, or bone marrow problems.
- High Hematocrit (Polycythemia): Can thicken the blood, increasing clot risk. It may cause headaches, dizziness, and blurred vision. It's often caused by dehydration but can also result from lung disease, smoking, or a bone marrow disorder called polycythemia vera.
- Key Factors: Your results are influenced by hydration, altitude, smoking, and pregnancy.
- Next Steps: Always discuss abnormal results with your healthcare provider, who will interpret them based on your overall health and may order follow-up tests.
Want the full explanation? Keep reading ↓
Hematocrit (Hct) is a vital component of a routine complete blood count (CBC) that provides crucial insights into a person's overall health. Often overlooked in favor of more commonly discussed parameters like hemoglobin, Hct plays a fundamental role in assessing the body's oxygen-carrying capacity. Essentially, hematocrit measures the volume percentage of red blood cells (RBCs) in your blood. It's a simple yet powerful indicator that can signal underlying medical conditions ranging from nutritional deficiencies to more serious chronic diseases.
Understanding your hematocrit levels and what they signify is an important step in managing your health. This article will delve into what constitutes normal hematocrit levels, provide a comprehensive chart for different populations, and explain how to interpret results that fall outside these ranges.
What is Hematocrit (Hct)?
Hematocrit, derived from the Greek words "haima" (blood) and "kritēs" (judge), literally means "to judge the blood." It quantifies the proportion of your blood that is made up of red blood cells. Red blood cells are essential for life, containing hemoglobin, a protein responsible for binding and transporting oxygen from the lungs to tissues and organs throughout the body, and carrying carbon dioxide back to the lungs.
When a blood sample is analyzed, it's typically spun in a centrifuge. This process separates the blood into its components: the plasma (the liquid portion) rises to the top, the white blood cells and platelets form a thin "buffy coat" in the middle, and the heavier red blood cells settle at the bottom. The hematocrit is then calculated as the percentage of the total blood volume occupied by these packed red blood cells. For a deeper dive into [what hematocrit measures] and its significance, refer to our dedicated article.
A healthy hematocrit level ensures that your body's tissues receive an adequate supply of oxygen to function correctly. Deviations from the normal range can indicate a variety of health issues, making Hct a critical diagnostic tool.
How is Hematocrit Measured?
Hematocrit is almost always measured as part of a complete blood count (CBC), one of the most common blood tests performed. A small blood sample, usually drawn from a vein in your arm, is sent to a laboratory for analysis. Modern automated analyzers can quickly and accurately determine the hematocrit, along with other blood cell parameters like red blood cell count, white blood cell count, and platelet count. While some older methods involved direct centrifugation and measurement, current techniques often calculate hematocrit from the red blood cell count and mean corpuscular volume (MCV), providing a highly precise result.
Normal Hematocrit Levels: The Chart
It's crucial to understand that "normal" hematocrit levels can vary based on several factors, including age, sex, altitude, and even hydration status. The ranges provided below are general guidelines, and individual laboratory reference ranges may differ slightly. Always interpret your results in consultation with a healthcare professional, as they can take into account your personal health history and other clinical findings.
Here is a chart outlining typical normal hematocrit ranges for different populations:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 40-54 | % | Varies by lab & altitude |
| Adult Women | 36-48 | % | Lower during menstruation or pregnancy |
| Children (Age-Dependent) | 30-44 | % | Ranges vary significantly by age; consult specific pediatric charts |
| Newborns | 45-61 | % | Higher due to fetal hemoglobin and physiological adjustments post-birth |
| Pregnant Women | 30-39 | % | Physiologically lower due to increased plasma volume (hemodilution) |
Key Considerations for the Chart:
- Units: Hematocrit is typically reported as a percentage (%). Sometimes it may be reported as a fraction (L/L), where 0.40 L/L is equivalent to 40%.
- Laboratory Variation: Reference ranges can vary slightly between different laboratories due to different equipment, techniques, and populations used to establish their "normal" values.
- Individual Variation: What is normal for one individual might be slightly different for another, even within the same demographic. Your doctor will consider your baseline and overall health picture.
- Altitude: People living at high altitudes often have naturally higher hematocrit levels to compensate for lower oxygen availability.
Interpreting Hematocrit Results
Understanding whether your hematocrit is too high or too low is the first step. The next is to understand what these deviations might signify.
Low Hematocrit: Anemia and Its Causes
A hematocrit level that falls below the normal range is often an indicator of anemia. Anemia is a condition characterized by a reduced number of healthy red blood cells or a decreased amount of hemoglobin, leading to insufficient oxygen delivery to the body's tissues. Symptoms of anemia can include fatigue, weakness, pale skin, shortness of breath, dizziness, cold hands and feet, and headaches.
Common causes of low hematocrit include:
- Iron Deficiency Anemia: This is the most common type of anemia worldwide. Iron is essential for hemoglobin production. Without enough iron, the body cannot produce sufficient hemoglobin, leading to smaller, paler red blood cells. Causes include inadequate dietary iron intake, chronic blood loss (e.g., heavy menstrual periods, gastrointestinal bleeding from ulcers or polyps), and impaired iron absorption.
- Vitamin Deficiencies:
- Vitamin B12 Deficiency (Megaloblastic Anemia): Vitamin B12 is crucial for red blood cell maturation. A deficiency can lead to the production of abnormally large, immature red blood cells (macrocytic anemia). This can be caused by poor dietary intake (especially in vegetarians/vegans), malabsorption issues (e.g., pernicious anemia, Crohn's disease), or certain medications.
- Folate Deficiency: Similar to B12, folate (folic acid) is vital for DNA synthesis in red blood cells. Deficiency can also lead to megaloblastic anemia. Causes include inadequate diet, alcoholism, and certain medications.
- Chronic Diseases: Kidney disease, cancer, inflammatory diseases (like rheumatoid arthritis or Crohn's disease), and chronic infections can suppress red blood cell production in the bone marrow, leading to anemia of chronic disease.
- Bone Marrow Disorders: Conditions affecting the bone marrow, where red blood cells are produced, can impair their production. Examples include aplastic anemia, myelodysplastic syndromes, and leukemia.
- Blood Loss: Acute or chronic bleeding can lead to a significant drop in red blood cell count and, consequently, hematocrit. This can range from trauma and surgery to internal bleeding that might not be immediately obvious.
- Hemolysis (Red Blood Cell Destruction): Certain conditions cause red blood cells to be destroyed prematurely. Examples include autoimmune hemolytic anemia, genetic disorders like sickle cell anemia or thalassemia, and reactions to certain medications or infections.
- Overhydration: An increase in the fluid portion (plasma) of the blood can dilute the red blood cells, leading to a falsely low hematocrit reading, even if the absolute number of red blood cells is normal. This is often seen in conditions like congestive heart failure or excessive intravenous fluid administration.
- Pregnancy: During pregnancy, a woman's blood volume increases significantly, with plasma volume increasing more than red blood cell mass. This physiological "dilution" often results in a slightly lower hematocrit, which is generally considered normal.
High Hematocrit: Polycythemia and Its Causes
A hematocrit level above the normal range is known as polycythemia or erythrocytosis. This means there is an abnormally high concentration of red blood cells in the blood. A high hematocrit can make the blood thicker, increasing its viscosity. Thicker blood flows less easily through blood vessels, raising the risk of blood clots, strokes, heart attacks, and other cardiovascular complications. Symptoms can include headache, dizziness, blurred vision, fatigue, shortness of breath, redness of the skin, and itching (especially after a hot bath).
Common causes of high hematocrit include:
- Dehydration: This is the most common cause of a transiently high hematocrit. When the body is dehydrated, the plasma volume decreases, concentrating the red blood cells and leading to a falsely elevated hematocrit reading. Once rehydrated, the hematocrit usually returns to normal.
- Polycythemia Vera (PV): This is a rare, chronic myeloproliferative disorder where the bone marrow produces too many red blood cells (and often white blood cells and platelets) independently of the body's needs. It is a serious condition that requires ongoing medical management.
- Chronic Hypoxia (Low Oxygen Levels): When the body consistently receives insufficient oxygen, it compensates by producing more red blood cells to try and increase oxygen-carrying capacity. Conditions that cause chronic hypoxia include:
- Chronic Obstructive Pulmonary Disease (COPD) and other lung diseases: Impaired lung function leads to poor oxygen exchange.
- Congenital heart disease: Structural heart defects can lead to inadequate oxygenation of the blood.
- High altitude living: Lower atmospheric oxygen pressure at high altitudes triggers increased RBC production.
- Sleep apnea: Intermittent drops in oxygen levels during sleep.
- Heavy smoking: Carbon monoxide in cigarette smoke reduces the oxygen-carrying capacity of hemoglobin, leading the body to produce more red blood cells to compensate.
- Kidney Disease/Tumors: The kidneys produce erythropoietin (EPO), a hormone that stimulates red blood cell production. Certain kidney diseases or tumors (e.g., renal cell carcinoma) can produce excess EPO, leading to increased red blood cell production.
- Other Tumors: Rarely, other tumors can produce EPO or EPO-like substances, causing secondary polycythemia.
- Testosterone Use: Exogenous testosterone (e.g., for hormone replacement therapy) can stimulate red blood cell production and lead to elevated hematocrit levels.
Factors Affecting Hematocrit Levels
Beyond specific diseases, several physiological and lifestyle factors can influence hematocrit levels:
- Age: Newborns have higher Hct, which then drops and gradually increases throughout childhood and adulthood.
- Sex: Adult men typically have higher Hct levels than adult women due to hormonal differences (androgens stimulate erythropoiesis) and menstrual blood loss in women.
- Hydration Status: As mentioned, dehydration falsely elevates Hct, while overhydration can falsely lower it. This is a common and often reversible cause of abnormal readings.
- Altitude: Living at high altitudes naturally increases Hct to adapt to lower oxygen.
- Smoking: Chronic smoking often leads to higher Hct due to carbon monoxide exposure and chronic hypoxia.
- Pregnancy: Normal physiological hemodilution results in lower Hct.
- Medications: Some medications can affect red blood cell production or fluid balance, impacting Hct.
- Recent Blood Transfusion: Can temporarily increase Hct.
- Recent Blood Donation: Can temporarily decrease Hct.
When to Be Concerned and Actionable Advice
An abnormal hematocrit reading is a signal, not a diagnosis in itself. It prompts further investigation to uncover the underlying cause.
If your hematocrit is low:
- Consult your doctor: They will likely order additional tests, such as a complete iron panel, vitamin B12 and folate levels, and a peripheral blood smear to examine the red blood cells more closely.
- Review your diet: Ensure adequate intake of iron-rich foods (red meat, poultry, fish, beans, lentils, spinach), vitamin B12 (animal products, fortified foods), and folate (leafy greens, fruits, nuts).
- Monitor symptoms: Pay attention to persistent fatigue, dizziness, or shortness of breath.
If your hematocrit is high:
- Consult your doctor: Further evaluation may include tests for erythropoietin levels, genetic testing for polycythemia vera, and assessment of lung and heart function.
- Stay hydrated: If dehydration is suspected, increasing fluid intake can help normalize Hct.
- Address lifestyle factors: If you smoke, quitting is crucial. If sleep apnea is suspected, seek medical evaluation.
- Monitor symptoms: Be aware of headaches, dizziness, or any signs of clotting.
The Importance of Context
It's vital to remember that a hematocrit result is just one piece of a larger puzzle. A healthcare provider will always interpret your hematocrit in the context of your overall medical history, physical examination, other blood test results (especially other components of the CBC like hemoglobin, red blood cell count, and red blood cell indices), and any symptoms you may be experiencing. For example, a low hematocrit might be considered normal for a pregnant woman, but a cause for concern in an adult man. Similarly, a slightly elevated hematocrit in someone living at high altitude might be physiological, whereas the same value in someone at sea level could indicate a problem.
Never attempt to self-diagnose or self-treat based solely on a single lab value. Always seek professional medical advice for interpretation and management of your hematocrit levels.
Conclusion
Hematocrit is a straightforward yet profoundly informative measure of the proportion of red blood cells in your blood. It serves as a critical indicator of your body's oxygen-carrying capacity and can be an early warning sign for a wide array of underlying health conditions, from nutritional deficiencies to more serious chronic diseases. While understanding the normal ranges for different populations is helpful, the true value of a hematocrit test lies in its interpretation by a qualified healthcare professional who can consider all aspects of your health. Regular check-ups and open communication with your doctor are key to ensuring your hematocrit levels, and your overall health, remain in optimal balance.
Frequently Asked Questions
What is the most common cause of abnormal Hematocrit (Hct) levels?
The most common cause of a low Hematocrit (anemia) is iron deficiency, often due to inadequate dietary intake or chronic blood loss (e.g., heavy menstrual periods, gastrointestinal bleeding). For a high Hematocrit (polycythemia), the most frequent cause is dehydration. When the body lacks sufficient fluid, the blood becomes more concentrated, leading to a falsely elevated hematocrit reading. Other common causes of high Hct include chronic lung diseases and living at high altitudes, which lead to chronic low oxygen levels.
How often should I get my Hematocrit (Hct) tested?
The frequency of Hct testing depends on your age, health status, and any existing medical conditions. For healthy adults, it's typically part of a routine complete blood count (CBC) during an annual physical examination. If you have a chronic condition that affects blood counts (e.g., kidney disease, cancer, inflammatory bowel disease) or are undergoing treatment that might impact red blood cell production (e.g., chemotherapy), your doctor may recommend more frequent testing, ranging from every few weeks to every few months, to monitor your condition and treatment effectiveness. If you experience symptoms of anemia or polycythemia, your doctor may order an Hct test immediately.
Can lifestyle changes improve my Hematocrit (Hct) levels?
Yes, lifestyle changes can significantly impact and often improve Hematocrit levels, especially when the abnormalities are related to diet, hydration, or certain habits.
- For low Hct (anemia): Increasing dietary intake of iron-rich foods (red meat, poultry, fish, beans, lentils, fortified cereals), vitamin B12 (animal products, fortified foods), and folate (leafy greens, fruits) can help. Avoiding excessive caffeine or tea with meals, which can inhibit iron absorption, and consuming vitamin C-rich foods to enhance iron absorption are also beneficial. Addressing any underlying blood loss is crucial.
- For high Hct (polycythemia): The most impactful lifestyle change is maintaining adequate hydration by drinking plenty of water throughout the day. If you smoke, quitting smoking is vital, as it's a major cause of chronic hypoxia and elevated Hct. For individuals living at high altitudes, the elevated Hct is often a natural adaptation, but managing other risk factors for cardiovascular disease becomes even more important. Consulting with a healthcare provider is essential to determine the specific cause and appropriate lifestyle adjustments.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.