High Hemoglobin Levels: Dehydration, Smoking & Polycythemia
Direct answer: High hemoglobin means you have an excess of oxygen-carrying protein in your red blood cells, often found on a routine blood test. This can be caused by temporary factors like dehydration, chronic conditions like smoking or lung disease, or a rare blood disorder called polycythemia vera. The elevated level can thicken your blood, increasing the risk of clots, so it's important to identify the underlying cause with your doctor.
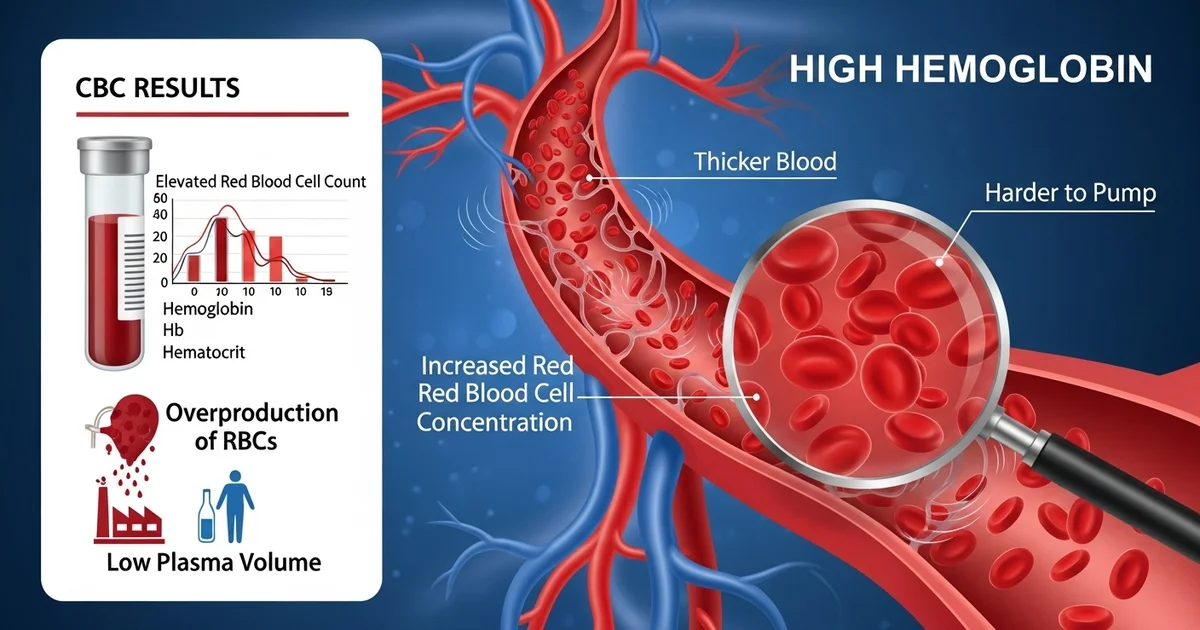
TL;DR High hemoglobin (Hb) means you have an increased concentration of red blood cells, which can make your blood thicker and harder to pump. This is often discovered during a routine Complete Blood Count (CBC). While sometimes temporary and easily fixed, it can also signal a more serious underlying health issue that requires medical attention. The main goal of diagnosis is to figure out why your body is either overproducing red blood cells or why your blood plasma volume is low, making the cells seem more concentrated.
- Dehydration: The most common temporary cause. When you're dehydrated, the liquid part of your blood (plasma) decreases, making your red blood cells more concentrated. Rehydrating usually resolves this.
- Smoking & Low Oxygen: Smoking introduces carbon monoxide into your blood, which reduces oxygen delivery. To compensate, your body produces more red blood cells. Other conditions causing low oxygen, like COPD or living at high altitude, have a similar effect.
- Polycythemia Vera (PV): A rare bone marrow cancer where the body produces too many red blood cells without proper regulation. This is a serious condition that increases the risk of blood clots, stroke, and heart attack.
- Symptoms: Many people have no symptoms. When they occur, they can include headaches, dizziness, fatigue, blurred vision, and sometimes itching, especially after a warm shower.
- What to Do: If your blood test shows high hemoglobin, your doctor will investigate further. This may involve checking for dehydration, measuring oxygen levels, and testing for the JAK2 gene mutation associated with Polycythemia Vera.
Want the full explanation? Keep reading ↓
Hemoglobin (Hb) is a critical protein found within red blood cells, playing an indispensable role in oxygen transport throughout the body. When hemoglobin levels are elevated above the normal range, it’s a condition known as high hemoglobin, or erythrocytosis. While sometimes a benign finding, high hemoglobin can also signal underlying health issues ranging from simple dehydration to more serious conditions like chronic lung disease or a bone marrow disorder. Understanding the potential causes, such as dehydration, smoking, and polycythemia, is crucial for proper diagnosis and management.
What is Hemoglobin?
At its core, hemoglobin is the oxygen-carrying component of your red blood cells. This iron-rich protein binds to oxygen in the lungs and releases it into tissues throughout the body, ensuring every cell receives the oxygen it needs to function. It also plays a role in transporting carbon dioxide back to the lungs to be exhaled. For a deeper dive into its vital functions, you can read our detailed article on [what is hemoglobin and its function in red blood cells].
When hemoglobin levels are high, it means there is an increased concentration of red blood cells in the blood, or a reduced plasma volume making the existing red blood cells appear more concentrated. This can lead to a thicker, more viscous blood, increasing the risk of blood clots and other complications.
Understanding High Hemoglobin Levels
High hemoglobin levels are typically identified through a Complete Blood Count (CBC), a routine blood test that measures various components of your blood, including red blood cells, white blood cells, and platelets. An elevated hemoglobin value often correlates with an elevated red blood cell count (erythrocytosis) and hematocrit (the percentage of blood volume occupied by red blood cells).
The body tightly regulates red blood cell production, primarily through a hormone called erythropoietin (EPO), produced by the kidneys. When oxygen levels in the blood are low (hypoxia), the kidneys release more EPO, stimulating the bone marrow to produce more red blood cells and, consequently, more hemoglobin. This is a natural adaptive response, but sustained or excessive stimulation can lead to abnormally high levels.
Normal Hemoglobin Reference Ranges
Hemoglobin levels vary based on age, sex, and other factors. It's important to compare your results against established reference ranges. You can learn more about these variations in our article on [hemoglobin normal range by age and sex].
Here’s a general guide to normal hemoglobin reference ranges:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 13.5-17.5 | g/dL | Higher levels often seen in athletes |
| Adult Women | 12.0-15.5 | g/dL | Lower in premenopausal due to menstruation |
| Children | 11.0-16.0 | g/dL | Highly age-dependent; newborns higher |
| Pregnant Women | 11.0-14.0 | g/dL | Lower due to hemodilution in later stages |
Note: These ranges are general guidelines and may vary slightly between different laboratories. Your healthcare provider will interpret your results in the context of your overall health.
Key Causes of High Hemoglobin
High hemoglobin levels can be broadly categorized into two types: relative polycythemia and absolute polycythemia. Relative polycythemia occurs when the plasma volume decreases, making the red blood cells appear more concentrated, even if the absolute number of red blood cells hasn't increased. Absolute polycythemia involves an actual increase in the total red blood cell mass.
Dehydration: A Common Cause of Relative Polycythemia
Dehydration is one of the most frequent causes of a temporarily elevated hemoglobin level. When your body loses more fluids than it takes in, the volume of plasma (the liquid component of blood) decreases. This makes the blood appear thicker and more concentrated, leading to a higher concentration of red blood cells and hemoglobin per unit of blood volume. This is an example of relative polycythemia or hemoconcentration.
- How it works: Imagine a cup of red cordial. If you pour out some water, the remaining cordial becomes more concentrated. Similarly, when you're dehydrated, the total number of red blood cells might not change, but because there's less fluid in your blood, the proportion of red blood cells (and thus hemoglobin) appears higher.
- Symptoms: Thirst, dry mouth, infrequent urination, fatigue, dizziness, and dark urine.
- Diagnosis: Often suspected based on clinical signs and confirmed by blood tests showing elevated hemoglobin/hematocrit that normalizes with rehydration.
- Management: Rehydration by drinking plenty of fluids is typically sufficient to correct high hemoglobin caused by dehydration. In severe cases, intravenous fluids may be necessary.
Smoking and Chronic Hypoxia: Stimulating Red Blood Cell Production
Chronic hypoxia, or persistently low oxygen levels in the blood, is a potent stimulus for red blood cell production. The body perceives low oxygen as a threat and responds by producing more red blood cells to enhance oxygen-carrying capacity.
Smoking
Cigarette smoking is a significant cause of chronic hypoxia. Carbon monoxide (CO) in cigarette smoke binds to hemoglobin with an affinity much higher than oxygen (about 200-250 times stronger), forming carboxyhemoglobin. This effectively reduces the amount of hemoglobin available to carry oxygen to tissues, creating a state of "functional anemia" or hypoxia, even if the total hemoglobin count is normal or high.
- How it works: To compensate for the reduced oxygen delivery caused by carboxyhemoglobin and damaged lung function, the kidneys release more erythropoietin (EPO). This increased EPO stimulates the bone marrow to produce more red blood cells, leading to elevated hemoglobin and hematocrit levels.
- Symptoms: Smokers with high hemoglobin may experience symptoms related to their underlying lung disease (e.g., chronic cough, shortness of breath) and symptoms of hyperviscosity (headache, dizziness).
- Diagnosis: Elevated carboxyhemoglobin levels can confirm smoking as a contributing factor.
- Management: Smoking cessation is the most effective intervention. This not only reduces carboxyhemoglobin levels but also improves lung function over time, allowing the body to reduce its compensatory red blood cell production.
Other Causes of Chronic Hypoxia
Beyond smoking, other conditions can cause chronic hypoxia and lead to high hemoglobin:
- Chronic Obstructive Pulmonary Disease (COPD): Conditions like emphysema and chronic bronchitis impair the lungs' ability to exchange gases efficiently, leading to persistent low oxygen levels.
- Sleep Apnea: Repeated episodes of breathing cessation during sleep cause intermittent hypoxia, which can stimulate EPO production.
- High Altitude Living: Individuals living at high altitudes naturally have lower atmospheric oxygen pressure, prompting their bodies to produce more red blood cells to adapt. This is a physiological and usually benign adaptation.
- Congenital Heart Disease: Certain heart defects can lead to inadequate oxygenation of the blood.
Polycythemia Vera: A Primary Bone Marrow Disorder
Polycythemia Vera (PV) is a type of myeloproliferative neoplasm (MPN), a rare, chronic blood cancer that originates in the bone marrow. In PV, the bone marrow produces too many red blood cells, and often too many white blood cells and platelets, independently of EPO regulation. This is a form of absolute polycythemia.
- Pathophysiology: PV is almost always associated with a mutation in the JAK2 gene (specifically, JAK2 V617F). This mutation causes the bone marrow stem cells to overproduce blood cells even when EPO levels are normal or low. The excess red blood cells significantly increase blood viscosity, leading to a higher risk of complications.
- Symptoms:
- Hyperviscosity symptoms: Headaches, dizziness, fatigue, blurred vision, tinnitus (ringing in the ears).
- Thrombotic events: Blood clots are a major concern, leading to strokes, heart attacks, deep vein thrombosis (DVT), and pulmonary embolism (PE).
- Erythromelalgia: Burning pain and redness in the hands and feet.
- Pruritus: Itching, especially after a warm bath or shower (aquagenic pruritus).
- Splenomegaly: Enlarged spleen due to increased blood cell production and sequestration.
- Diagnosis: Diagnosis involves a combination of:
- Elevated hemoglobin/hematocrit: Persistently high levels.
- Low or normal EPO levels: Differentiating it from secondary polycythemia.
- JAK2 gene mutation testing: The presence of JAK2 V617F is a key diagnostic marker.
- Bone marrow biopsy: May be performed to confirm the diagnosis and assess bone marrow cellularity.
- Complications: The primary risks are thrombotic events (blood clots), which can be life-threatening. Over time, PV can also transform into myelofibrosis (scarring of the bone marrow) or, rarely, acute myeloid leukemia.
- Treatment: Management aims to reduce the risk of complications and control symptoms:
- Phlebotomy: Regular removal of blood (similar to blood donation) to reduce red blood cell mass and normalize hematocrit.
- Low-dose aspirin: To reduce the risk of blood clots.
- Myelosuppressive agents: Medications like hydroxyurea or ruxolitinib may be used to suppress bone marrow production of blood cells, especially in high-risk patients or those intolerant to phlebotomy.
Other Causes of Absolute Polycythemia (Secondary Polycythemia)
While PV is a primary bone marrow disorder, secondary polycythemia refers to an increased red blood cell mass due to an identifiable underlying condition that drives EPO production.
- Kidney Disease: Rarely, certain kidney conditions or tumors (e.g., renal cell carcinoma, renal cysts) can inappropriately produce high amounts of EPO.
- Androgen Use: Anabolic steroids (androgens) can stimulate EPO production.
- Genetic Conditions: Very rare genetic mutations can lead to increased EPO sensitivity or production, or alter hemoglobin's oxygen-binding affinity.
Symptoms Associated with High Hemoglobin
Regardless of the cause, high hemoglobin levels can lead to symptoms due to increased blood viscosity, which makes blood flow sluggishly, and potentially reduced oxygen delivery despite more red blood cells. Common symptoms include:
- Headaches
- Dizziness or lightheadedness
- Fatigue
- Blurred vision or visual disturbances
- Tinnitus (ringing in the ears)
- Reddish or flushed complexion (plethora)
- Itching (pruritus), especially after bathing
- Pain or numbness in the hands and feet (erythromelalgia)
- Shortness of breath
- Weakness
These symptoms are non-specific and can overlap with many other conditions, emphasizing the need for medical evaluation.
Diagnosis of High Hemoglobin
When high hemoglobin is detected on a CBC, further investigation is warranted. The diagnostic process typically involves:
- Repeat CBC: To confirm persistent elevation.
- Detailed Medical History and Physical Exam: To identify risk factors like smoking, dehydration, living at high altitude, or symptoms suggestive of underlying conditions.
- Erythropoietin (EPO) Level Measurement:
- Low EPO: Suggests a primary bone marrow disorder like Polycythemia Vera.
- High EPO: Points towards secondary polycythemia, where the body is appropriately responding to hypoxia or an EPO-producing tumor.
- Oxygen Saturation Measurement: To assess for chronic hypoxia.
- Imaging Studies: Such as chest X-ray, CT scan, or ultrasound, to evaluate lung or kidney conditions that might cause hypoxia or produce EPO.
- Genetic Testing: For JAK2 mutation if Polycythemia Vera is suspected.
- Bone Marrow Biopsy: May be necessary to confirm Polycythemia Vera or other bone marrow disorders.
Management and Treatment
Treatment for high hemoglobin levels is entirely dependent on the underlying cause.
- For Dehydration: Rehydration is the primary treatment. Ensuring adequate fluid intake is crucial.
- For Smoking/Chronic Hypoxia:
- Smoking cessation is paramount for smokers.
- Management of underlying conditions like COPD, sleep apnea, or heart disease is essential. This may involve bronchodilators, oxygen therapy, CPAP machines, or cardiac medications.
- For Polycythemia Vera:
- Phlebotomy to reduce red blood cell mass.
- Low-dose aspirin to prevent clots.
- Myelosuppressive drugs (e.g., hydroxyurea, ruxolitinib) for high-risk patients or those with severe symptoms.
- For Secondary Polycythemia due to other causes: Treatment focuses on addressing the root cause, such as removing an EPO-producing tumor or managing kidney disease.
Actionable Advice: If your hemoglobin levels are found to be high, it's crucial to consult with a healthcare professional. Do not attempt to self-diagnose or self-treat. Your doctor will conduct the necessary tests to determine the cause and recommend the most appropriate course of action. Maintaining a healthy lifestyle, including adequate hydration, avoiding smoking, and managing chronic health conditions, can play a significant role in maintaining balanced hemoglobin levels.
Conclusion
High hemoglobin levels, or erythrocytosis, are a finding that warrants medical attention. While sometimes a simple reflection of dehydration, it can also be a sign of chronic hypoxia from conditions like smoking or lung disease, or indicate a more serious hematological disorder such as Polycythemia Vera. Accurate diagnosis of the underlying cause is essential for effective management and to mitigate the risks associated with increased blood viscosity, especially the heightened risk of blood clots. Regular check-ups and open communication with your healthcare provider are key to understanding and managing your hemoglobin levels for optimal health.
Frequently Asked Questions
What is the most common cause of abnormal Hemoglobin (Hb) levels?
The most common cause of abnormal hemoglobin levels overall is actually low hemoglobin, which is indicative of anemia. Anemia affects a vast number of people worldwide, often due to iron deficiency, chronic disease, or blood loss. When considering high hemoglobin levels specifically, dehydration is arguably the most common cause, as it leads to relative polycythemia which resolves with rehydration. Beyond dehydration, chronic conditions causing hypoxia (like smoking or lung disease) are also very common causes of elevated hemoglobin.
How often should I get my Hemoglobin (Hb) tested?
The frequency of hemoglobin testing depends on your age, health status, and any existing medical conditions. For healthy adults without specific risk factors or symptoms, a hemoglobin test is typically part of a routine Complete Blood Count (CBC) performed during an annual physical exam, or every few years as recommended by your doctor. If you have symptoms suggestive of anemia or high hemoglobin, a chronic condition (like kidney disease, heart disease, or a known blood disorder), or are undergoing certain treatments, your doctor may recommend more frequent testing, ranging from every few months to annually. Always follow your healthcare provider's specific recommendations.
Can lifestyle changes improve my Hemoglobin (Hb) levels?
Yes, lifestyle changes can significantly impact hemoglobin levels, particularly when they are outside the normal range due to preventable causes. For high hemoglobin, stopping smoking is one of the most impactful changes, as it directly addresses chronic hypoxia and reduces carboxyhemoglobin. Maintaining adequate hydration by drinking enough water throughout the day can prevent and correct relative polycythemia due to dehydration. For individuals with high hemoglobin secondary to conditions like sleep apnea or obesity, weight management and adhering to prescribed treatments (e.g., CPAP for sleep apnea) can help normalize oxygen levels and reduce the need for compensatory red blood cell production. While lifestyle changes are crucial, it's important to remember that they are not a substitute for medical evaluation and treatment, especially for conditions like Polycythemia Vera.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.