Hemoglobin (Hb): Understanding Your Blood Test Results
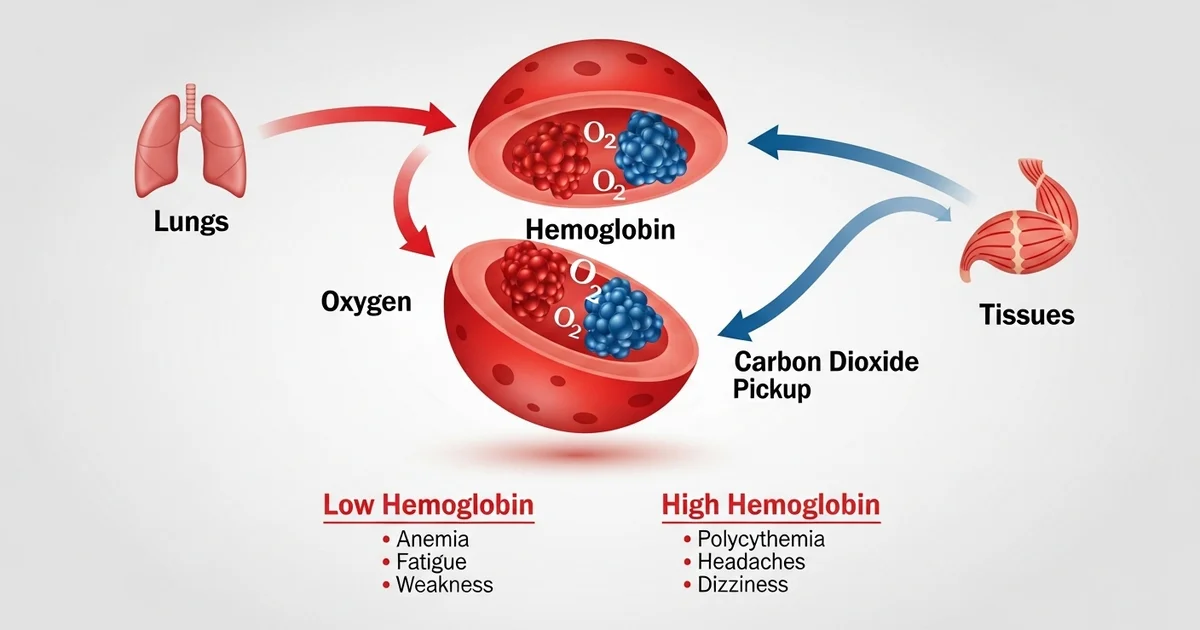
Direct answer: Hemoglobin (Hb) is a protein in your red blood cells that carries oxygen from the lungs to your body's tissues. It's a key measurement in a complete blood count (CBC) used to diagnose conditions like anemia (low Hb) or polycythemia (high Hb).
TL;DR Hemoglobin is the essential protein in red blood cells responsible for transporting oxygen throughout your body. It picks up oxygen in the lungs and delivers it to your tissues, then helps carry carbon dioxide back. Your hemoglobin level, measured in a complete blood count (CBC), is a critical indicator of your overall health. Levels that are too low or too high can signal underlying medical conditions that need attention.
- Hemoglobin's main job is to carry oxygen, which is vital for energy production in your cells.
- Low hemoglobin is called anemia and can cause fatigue, weakness, and shortness of breath.
- High hemoglobin, known as polycythemia, can thicken your blood and increase the risk of clots.
- Common causes of low hemoglobin include iron deficiency, vitamin deficiencies, and chronic blood loss.
- Dehydration, smoking, and living at high altitudes can cause high hemoglobin levels.
- Normal hemoglobin ranges vary based on age, sex, and pregnancy status.
- Your doctor uses this test to diagnose health issues, monitor chronic conditions, and assess overall health.
Want the full explanation? Keep reading ↓
Hemoglobin (Hb) is an indispensable protein found within red blood cells (erythrocytes) that serves as the primary transporter of oxygen from the lungs to the body's tissues and carbon dioxide from the tissues back to the lungs. Its critical role in sustaining life underscores its importance in clinical medicine, making it a routine measurement in a complete blood count (CBC) to assess overall health and diagnose various conditions. Understanding hemoglobin's structure, function, and the factors influencing its levels is fundamental to comprehending many physiological processes and common diseases.
What is Hemoglobin? The Molecular Structure
Hemoglobin is a complex metalloprotein, typically consisting of four protein subunits. Each subunit is composed of two main parts:
- Heme Group: This is the non-protein component, a porphyrin ring structure containing a single iron atom (Fe2+) at its center. It is this iron atom that reversibly binds to oxygen. The ferrous (Fe2+) state of iron is crucial for oxygen binding; if iron is oxidized to the ferric (Fe3+) state, it forms methemoglobin, which cannot bind oxygen efficiently.
- Globin Chains: These are the protein components, typically two pairs of polypeptide chains. In adults, the most common type of hemoglobin is Hemoglobin A (HbA), which consists of two alpha (α) globin chains and two beta (β) globin chains (α2β2). Other types of hemoglobin exist:
- Hemoglobin A2 (HbA2): Composed of two alpha and two delta (δ) chains (α2δ2), present in small amounts in adults.
- Hemoglobin F (HbF): Fetal hemoglobin, composed of two alpha and two gamma (γ) chains (α2γ2). HbF has a higher affinity for oxygen than HbA, which facilitates oxygen transfer from the mother to the fetus during pregnancy. HbF levels decrease significantly after birth but can reappear in certain blood disorders.
The intricate three-dimensional structure of hemoglobin allows it to efficiently bind and release oxygen. When oxygen binds to one heme group, it induces a conformational change in the protein, increasing the affinity of the other heme groups for oxygen. This phenomenon, known as cooperativity, ensures efficient oxygen loading in the lungs where oxygen concentration is high, and efficient unloading in the tissues where oxygen concentration is low.
The Crucial Function of Hemoglobin: Oxygen Transport
The primary and most vital function of hemoglobin is the transport of oxygen. This process is meticulously regulated to meet the metabolic demands of the body.
Oxygen Binding in the Lungs
As red blood cells pass through the capillaries of the lungs, where the partial pressure of oxygen is high:
- Oxygen molecules diffuse from the alveoli into the red blood cells.
- Each of the four heme groups in a hemoglobin molecule rapidly binds to one oxygen molecule, forming oxyhemoglobin.
- This binding is reversible, meaning oxygen can be released when needed.
- The high oxygen affinity in the lungs ensures maximum oxygen saturation.
Oxygen Release in Tissues
Upon reaching the peripheral tissues, where metabolic activity is high and the partial pressure of oxygen is low:
- Hemoglobin undergoes a conformational change, decreasing its affinity for oxygen.
- Oxygen molecules are released from oxyhemoglobin and diffuse out of the red blood cells into the surrounding tissue cells, where they are used for cellular respiration (energy production).
- Several factors facilitate this release, including:
- Lower pH (higher acidity): Tissues producing more carbon dioxide (a byproduct of metabolism) become more acidic, which promotes oxygen release (Bohr effect).
- Higher temperature: Increased metabolic activity generates heat, which also reduces hemoglobin's oxygen affinity.
- Increased 2,3-bisphosphoglycerate (2,3-BPG): This molecule, produced by red blood cells, binds to hemoglobin and stabilizes its deoxygenated state, further enhancing oxygen release in tissues.
Carbon Dioxide Transport (Minor Role)
While hemoglobin is primarily known for oxygen transport, it also plays a secondary role in carbon dioxide transport.
- Approximately 10-20% of carbon dioxide produced by tissues binds directly to the amino groups of the globin chains, forming carbaminohemoglobin.
- The majority of carbon dioxide is transported in the blood as bicarbonate ions (HCO3-), a process facilitated by the enzyme carbonic anhydrase within red blood cells. Hemoglobin also acts as a buffer, helping to maintain blood pH by binding to hydrogen ions produced from carbonic acid dissociation.
Hemoglobin Synthesis and Red Blood Cell Life Cycle
The journey of hemoglobin begins in the bone marrow, the body's primary site for blood cell production.
Erythropoiesis and Hemoglobin Production
- Red blood cell production, known as erythropoiesis, is a complex process primarily regulated by the hormone erythropoietin (EPO), produced by the kidneys in response to low oxygen levels.
- Immature red blood cells (erythroblasts) in the bone marrow synthesize large quantities of hemoglobin. This process requires a steady supply of essential nutrients:
- Iron: Crucial for the synthesis of the heme group.
- Vitamin B12 (cobalamin) and Folate (Vitamin B9): Essential for DNA synthesis, which is required for cell division and maturation of red blood cell precursors.
- Amino acids: Building blocks for the globin protein chains.
- As red blood cells mature, they extrude their nucleus and other organelles, becoming biconcave discs devoid of a nucleus, which maximizes their surface area for gas exchange and allows them to navigate narrow capillaries.
Red Blood Cell Lifespan and Breakdown
- Mature red blood cells circulate in the bloodstream for approximately 100 to 120 days.
- As they age, their membranes become less flexible, and they are eventually recognized and removed from circulation by macrophages, primarily in the spleen, liver, and bone marrow.
- During this breakdown:
- The globin chains are broken down into amino acids, which are recycled.
- The iron from the heme group is salvaged and transported back to the bone marrow by a protein called transferrin to be reused in new hemoglobin synthesis.
- The porphyrin ring of the heme group is converted into bilirubin, a yellow pigment that is transported to the liver, conjugated, and excreted in bile.
Measuring Hemoglobin Levels: The CBC Test
Hemoglobin levels are routinely measured as part of a Complete Blood Count (CBC), one of the most common blood tests performed. A CBC provides a comprehensive overview of the different types of cells in the blood, including red blood cells, white blood cells, and platelets.
Why Hemoglobin is Measured
Measuring hemoglobin is critical for:
- Diagnosing Anemia: Low hemoglobin levels are the hallmark of anemia, indicating a reduced oxygen-carrying capacity of the blood.
- Diagnosing Polycythemia: High hemoglobin levels can indicate an overproduction of red blood cells, which can lead to increased blood viscosity and other health issues.
- Monitoring Treatment: Hemoglobin levels are monitored to assess the effectiveness of treatments for conditions like anemia (e.g., iron supplementation).
- Assessing Blood Loss: Significant blood loss, whether acute or chronic, will manifest as decreased hemoglobin.
- Evaluating Overall Health: Hemoglobin levels can be influenced by hydration status, chronic diseases, nutritional deficiencies, and other factors, providing insights into a patient's general well-being.
Units of Measurement
Hemoglobin concentration is typically reported in grams per deciliter (g/dL) or sometimes in millimoles per liter (mmol/L). The reference ranges vary based on age, sex, and other factors.
Understanding Hemoglobin Reference Ranges
Normal hemoglobin levels vary significantly among different populations due to physiological differences. It's crucial to interpret individual results in the context of these reference ranges, which are often provided by the laboratory performing the test. Deviations from these ranges can indicate underlying health conditions requiring further investigation.
Hemoglobin Reference Ranges
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 13.5 - 17.5 | g/dL | Generally higher due to testosterone |
| Adult Women (non-pregnant) | 12.0 - 15.5 | g/dL | Lower due to menstrual blood loss |
| Pregnant Women (2nd trimester) | 10.5 - 14.0 | g/dL | Physiologic hemodilution occurs |
| Children (6-12 years) | 11.0 - 15.0 | g/dL | Age-dependent, consult specific pediatric ranges |
| Infants (birth to 1 month) | 13.5 - 20.0 | g/dL | Higher at birth, decreases after 2-3 months |
Note: These ranges are approximate and can vary slightly between laboratories. Always refer to the specific reference ranges provided by the testing laboratory.
High Hemoglobin Levels (Polycythemia)
Elevated hemoglobin levels, a condition known as polycythemia or erythrocytosis, mean that the blood has an abnormally high concentration of red blood cells. This can lead to increased blood viscosity, making it thicker and more prone to clotting, which can raise the risk of strokes, heart attacks, and other cardiovascular events.
Causes of High Hemoglobin
- Dehydration: The most common cause of a transiently high hemoglobin is dehydration. When there is less fluid (plasma) in the blood, the concentration of red blood cells appears higher. This is often referred to as relative polycythemia.
- Chronic Hypoxia (Low Oxygen Levels): The body compensates for prolonged low oxygen by producing more red blood cells to enhance oxygen-carrying capacity. Conditions that cause chronic hypoxia include:
- Chronic Obstructive Pulmonary Disease (COPD)
- Sleep Apnea
- High Altitude Living
- Congenital Heart Disease
- Polycythemia Vera (PV): A rare, chronic myeloproliferative neoplasm where the bone marrow produces too many red blood cells, and often white blood cells and platelets, independently of erythropoietin regulation.
- Kidney Tumors or Cysts: These can sometimes produce excess erythropoietin, stimulating red blood cell production.
- Smoking: Smokers often have higher hemoglobin levels due to carbon monoxide exposure, which reduces oxygen delivery to tissues, prompting the body to produce more red blood cells as compensation.
Symptoms of High Hemoglobin
Symptoms can be vague and non-specific, including:
- Headaches
- Dizziness
- Fatigue
- Blurred vision
- Reddish or purple skin, especially in the face, hands, and feet
- Shortness of breath
- Splenomegaly (enlarged spleen) in conditions like polycythemia vera
Clinical Significance
High hemoglobin levels warrant investigation to determine the underlying cause. Treatment focuses on managing the primary condition and reducing the risk of complications like blood clots. This may involve therapeutic phlebotomy (blood letting) to reduce red blood cell mass, or medications to suppress bone marrow production in cases like polycythemia vera.
Low Hemoglobin Levels (Anemia)
Low hemoglobin levels, a condition known as anemia, indicate that the blood has a reduced capacity to carry oxygen, leading to insufficient oxygen delivery to the body's tissues. This is a very common condition with a wide range of causes.
Causes of Low Hemoglobin
Anemia can result from three main mechanisms: decreased red blood cell production, increased red blood cell destruction, or blood loss.
- Decreased Red Blood Cell Production:
- Iron Deficiency Anemia: The most common type of anemia worldwide. Insufficient iron leads to impaired heme synthesis. Causes include inadequate dietary intake, malabsorption, or chronic blood loss.
- Vitamin Deficiency Anemia (B12 and Folate): Deficiencies in these vitamins impair DNA synthesis, leading to the production of large, immature red blood cells (megaloblastic anemia).
- Anemia of Chronic Disease (ACD): Often seen in chronic infections, inflammatory diseases (e.g., rheumatoid arthritis, inflammatory bowel disease), or cancer. Inflammation interferes with iron utilization and erythropoietin production.
- Aplastic Anemia: Rare but severe condition where the bone marrow fails to produce enough blood cells.
- Kidney Disease: Impaired kidney function can lead to reduced erythropoietin production.
- Increased Red Blood Cell Destruction (Hemolytic Anemia):
- Genetic Conditions: Such as sickle cell anemia (abnormal beta-globin chains leading to crescent-shaped red blood cells that are fragile and block vessels) and thalassemia (impaired production of alpha or beta globin chains).
- Autoimmune Hemolytic Anemia: The immune system mistakenly attacks and destroys red blood cells.
- Drug-induced Hemolysis: Certain medications can trigger red blood cell destruction.
- Infections: Some infections can lead to hemolysis.
- Blood Loss:
- Acute Blood Loss: Trauma, surgery, or severe gastrointestinal bleeding.
- Chronic Blood Loss: Often subtle and prolonged, such as from peptic ulcers, hemorrhoids, heavy menstrual periods, or gastrointestinal cancers. This is a common cause of iron deficiency anemia.
Symptoms of Low Hemoglobin
Symptoms vary depending on the severity and duration of the anemia but commonly include:
- Fatigue and Weakness: Due to reduced oxygen delivery to muscles and organs.
- Shortness of Breath: Especially during exertion.
- Pale Skin, Gums, and Nail Beds: Reduced red blood cell count decreases the reddish tint of blood.
- Dizziness or Lightheadedness
- Headaches
- Cold Hands and Feet
- Chest Pain (severe cases)
- Fast or Irregular Heartbeat
- Pica (craving for non-food items like ice or dirt) in iron deficiency anemia.
Clinical Significance
Anemia requires prompt diagnosis and treatment to address the underlying cause and restore adequate oxygen-carrying capacity. Untreated anemia can lead to severe fatigue, impaired organ function, and increased risk of cardiovascular complications.
Actionable Advice and Maintaining Healthy Hemoglobin Levels
Maintaining healthy hemoglobin levels is vital for overall health and well-being. Here's actionable advice:
- Balanced Diet Rich in Iron:
- Heme Iron (highly absorbable): Found in animal products like red meat, poultry, fish, and liver.
- Non-Heme Iron (less absorbable): Found in plant-based foods such as lentils, beans, spinach, fortified cereals, tofu, and pumpkin seeds.
- Enhance Iron Absorption: Consume Vitamin C (citrus fruits, bell peppers, broccoli) with iron-rich meals, as it significantly boosts non-heme iron absorption. Avoid consuming iron-rich foods with calcium (dairy products) or tannins (tea, coffee) as they can inhibit iron absorption.
- Ensure Adequate Vitamin Intake:
- Vitamin B12: Found in animal products (meat, fish, dairy, eggs). Vegetarians and vegans may need fortified foods or supplements.
- Folate (Vitamin B9): Found in leafy green vegetables, fruits, nuts, beans, and fortified grains.
- Stay Hydrated: Drink plenty of water throughout the day to prevent dehydration, which can falsely elevate hemoglobin readings and impact overall blood volume.
- Manage Chronic Conditions: If you have a chronic disease (e.g., kidney disease, inflammatory bowel disease), work with your healthcare provider to manage it effectively, as these conditions can impact hemoglobin levels.
- Regular Medical Check-ups: Routine physical exams and blood tests, including a CBC, can help detect abnormal hemoglobin levels early, often before symptoms become severe.
- Avoid Smoking: Quitting smoking can help improve oxygen delivery and potentially normalize hemoglobin levels that were elevated due to chronic hypoxia.
- Limit Alcohol Intake: Excessive alcohol consumption can interfere with nutrient absorption and bone marrow function.
- When to Seek Medical Attention: If you experience persistent symptoms of anemia (e.g., severe fatigue, shortness of breath, dizziness) or polycythemia (e.g., headaches, dizziness, unexplained redness of skin), consult your doctor promptly. Self-treating with iron supplements without medical advice can be dangerous, as too much iron can be toxic.
Frequently Asked Questions
What is the most common cause of abnormal Hemoglobin (Hb) levels?
The most common cause of low hemoglobin is iron deficiency anemia. This occurs when the body lacks sufficient iron to produce adequate amounts of hemoglobin, leading to a reduced oxygen-carrying capacity of the blood. It can stem from insufficient dietary iron intake, poor absorption of iron, or chronic blood loss (e.g., heavy menstrual periods, gastrointestinal bleeding). For high hemoglobin, the most common cause is dehydration. When the body is dehydrated, the plasma volume decreases, making the concentration of red blood cells and hemoglobin appear artificially high. Other common causes of genuinely high hemoglobin involve the body compensating for chronic low oxygen levels (e.g., due to smoking, high altitude, or chronic lung diseases like COPD).
How often should I get my Hemoglobin (Hb) tested?
The frequency of hemoglobin testing depends on your individual health status, age, and risk factors.
- For healthy adults with no symptoms or known risk factors, a hemoglobin test is typically included as part of a routine complete blood count (CBC) during an annual physical exam or every few years as recommended by your doctor.
- For individuals with chronic conditions (e.g., kidney disease, chronic inflammatory diseases, cancer) or those taking medications that affect blood cell production, more frequent monitoring (e.g., every 3-6 months) may be necessary.
- Pregnant women are usually tested at their first prenatal visit and again in the second or third trimester to monitor for anemia, which is common during pregnancy.
- Individuals with a history of anemia or iron deficiency may require periodic testing to monitor treatment effectiveness and ensure levels remain stable.
- If you experience symptoms suggestive of anemia (fatigue, paleness, shortness of breath) or polycythemia (headaches, dizziness, redness), your doctor will likely order a hemoglobin test regardless of your last check-up.
Can lifestyle changes improve my Hemoglobin (Hb) levels?
Yes, lifestyle changes can significantly improve hemoglobin levels, especially in cases of nutritional deficiencies or lifestyle-related factors.
- Dietary Modifications: This is paramount for improving low hemoglobin due to iron, B12, or folate deficiencies. Incorporating iron-rich foods (red meat, poultry, fish, beans, lentils, fortified cereals), along with Vitamin C sources to enhance iron absorption, is crucial. For B12 deficiency, consuming animal products or fortified foods/supplements is essential.
- Hydration: For high hemoglobin levels caused by dehydration, simply increasing fluid intake can normalize hemoglobin concentration.
- Smoking Cessation: Quitting smoking can significantly improve oxygen delivery to tissues, reducing the body's need to compensate by overproducing red blood cells, thereby helping to lower elevated hemoglobin levels.
- Managing Chronic Conditions: Adhering to treatment plans for chronic diseases like kidney disease, inflammatory bowel disease, or sleep apnea can indirectly help maintain healthy hemoglobin levels by addressing the underlying cause of abnormal red blood cell production or destruction.
- Regular Exercise: While not a direct treatment for severe anemia, moderate exercise can improve overall cardiovascular health and blood circulation, which supports efficient oxygen transport. However, individuals with severe anemia should consult their doctor before starting an exercise regimen. It's important to consult with a healthcare professional to identify the specific cause of abnormal hemoglobin levels and receive personalized advice and treatment.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.