What is Folate (Vitamin B9)? Roles in Body & Pregnancy
Introduction
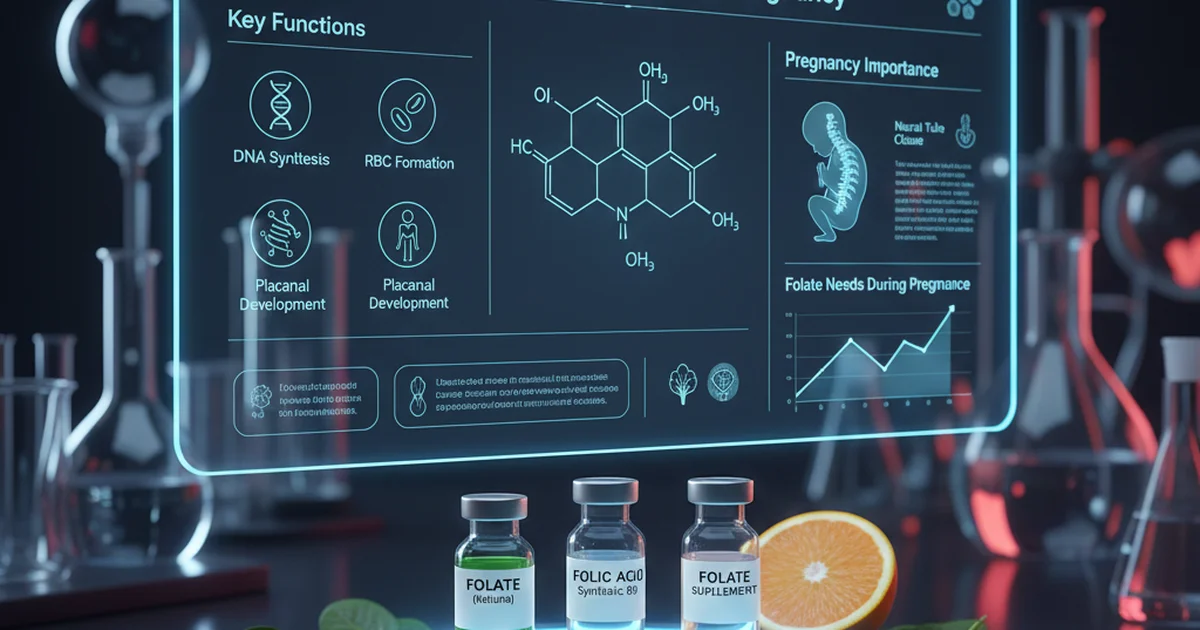
Folate, also known as vitamin B9, is a water‑soluble B‑vitamin that plays a central role in one‑carbon metabolism, DNA synthesis, and amino‑acid interconversion. The term “folate” refers to the collection of naturally occurring compounds found in foods (e.g., 5‑methyltetrahydrofolate, folic acid), whereas folic acid is the synthetic, oxidized form used in fortified foods and dietary supplements. Adequate folate status is essential for every cell in the body, but its importance is magnified during periods of rapid growth and cell division—most notably in pregnancy, where it supports neural‑tube closure, red‑blood‑cell formation, and placental development.
Biological Functions of Folate
| Function | Mechanism | Clinical Significance |
|---|---|---|
| DNA & RNA synthesis | Serves as a methyl donor for thymidine and purine production | Prevents megaloblastic anemia, supports tissue growth |
| Amino‑acid metabolism | Converts homocysteine to methionine via methionine synthase | Lowers homocysteine, reduces cardiovascular risk |
| Methylation reactions | Provides methyl groups for epigenetic regulation | Influences gene expression, neurodevelopment |
| Red blood cell formation | Supports erythropoiesis in the bone marrow | Deficiency → macrocytic anemia |
| Neural‑tube closure | Critical during weeks 3‑4 of gestation | Deficiency → spina bifida, anencephaly |
Dietary Sources & Bioavailability
Natural Food Sources
| Food Group | Typical Folate Content (µg DFE per serving) | Comments |
|---|---|---|
| Dark leafy greens (spinach, kale, collard greens) | 80–120 | High but sensitive to cooking |
| Legumes (lentils, chickpeas, black beans) | 150–200 | Excellent plant source; also protein‑rich |
| Citrus fruits & juices (orange, grapefruit) | 30–50 | Vitamin C improves folate stability |
| Avocado | 80 | Provides healthy fats that aid nutrient absorption |
| Asparagus, broccoli, Brussels sprouts | 50–80 | Best consumed lightly steamed |
| Whole grains (fortified wheat flour, quinoa) | 30–60 | Fortified versions contain synthetic folic acid |
Key point: Naturally occurring folates are primarily 5‑methyltetrahydrofolate (5‑MTHF), the bioactive form that circulates in plasma. They are moderately stable but can be lost during prolonged boiling or exposure to light.
Fortified Foods & Supplements
| Source | Folate Form | Typical Content (µg DFE) | Bioavailability |
|---|---|---|---|
| Enriched bread, cereals, pasta | Folic acid (synthetic) | 100–400 per serving | ~85–100 %, higher than natural folate |
| Prenatal vitamins | Folic acid (often 400–800 µg) + 5‑MTHF (optional) | 400–800 | Highly absorbable; recommended for women of childbearing age |
| Multivitamins (adult formulas) | Folic acid | 200–400 | Good for general population |
Why the difference? Folic acid, being a fully oxidized and stable molecule, is absorbed via the reduced folate carrier in the small intestine and then reduced to 5‑MTHF in the liver. This conversion is efficient in most individuals, yielding a higher bioavailability than food folates, which must first be liberated from the food matrix.
Factors Influencing Absorption
- Alcohol: Chronic intake impairs folate absorption and hepatic storage.
- Medications: Antiepileptics (phenytoin, carbamazepine), methotrexate, and trimethoprim can antagonize folate metabolism.
- Genetic polymorphisms: Variants in the MTHFR gene (e.g., C677T) reduce the conversion of folic acid to 5‑MTHF, potentially requiring supplementation with the active form.
- Gut health: Malabsorption syndromes (celiac disease, inflammatory bowel disease) lower folate uptake.
Reference Ranges
| Population | Test | Normal Range | Units | Notes |
|---|---|---|---|---|
| Adult Men | Serum folate | 3–20 | ng/mL | Reflects recent intake |
| Adult Women (non‑pregnant) | Serum folate | 3–20 | ng/mL | Slightly lower in premenopausal women |
| Pregnant Women (any trimester) | Serum folate | 4–24 | ng/mL | Target > 6 ng/mL to reduce neural‑tube risk |
| Children (1–12 y) | Serum folate | 2–15 | ng/mL | Age‑dependent; lower in toddlers |
| Adults | Red blood cell (RBC) folate | 140–628 | ng/mL | Indicates long‑term status; > 400 ng/mL optimal for pregnancy |
| Elderly (> 65 y) | Serum folate | 2–12 | ng/mL | May be reduced due to decreased dietary intake |
Clinical tip: Serum folate reflects short‑term intake (days), whereas RBC folate provides a 3‑month picture of tissue stores. For preconception counseling, RBC folate is the preferred marker.
Recommended Intakes
| Life Stage | Recommended Dietary Allowance (RDA) | Tolerable Upper Intake Level (UL) |
|---|---|---|
| Adults (both sexes) | 400 µg Dietary Folate Equivalents (DFE) | 1 000 µg folic acid (synthetic) |
| Pregnant women | 600 µg DFE | 1 000 µg folic acid |
| Lactating women | 500 µg DFE | 1 000 µg folic acid |
| Adolescents (14–18 y) | 400 µg DFE | 1 000 µg folic acid |
| Children (9–13 y) | 300 µg DFE | 300 µg folic acid |
| Infants (0–6 mo) | 65 µg DFE | No UL established |
Note: 1 µg DFE = 1 µg food folate = 0.6 µg folic acid from fortified foods or supplements.
Folate in Pregnancy
Why Folate Matters
- Neural‑tube closure occurs between days 21–28 post‑conception, often before a woman knows she is pregnant. Adequate folate reduces the risk of spina bifida and anencephaly by up to 70 %.
- DNA synthesis supports rapid fetal cell proliferation and placental growth.
- Homocysteine regulation protects maternal vascular health, decreasing the likelihood of preeclampsia.
Evidence‑Based Dosage
- Standard recommendation: 400–600 µg DFE daily for all women of childbearing age, beginning at least one month before conception and continuing through the first 12 weeks of gestation.
- High‑risk groups (history of neural‑tube defect, MTHFR C677T homozygosity, obesity, diabetes, antiepileptic therapy) may benefit from 4 mg (4 000 µg) daily folic acid under medical supervision.
Timing of Supplementation
| Period | Goal | Recommended Intake |
|---|---|---|
| Preconception (≥ 1 mo prior) | Build tissue stores | 400–800 µg DFE (synthetic folic acid) |
| First trimester | Neural‑tube protection | Continue 400–800 µg DFE |
| Second & third trimesters | Support fetal growth & maternal erythropoiesis | 600 µg DFE (often met by prenatal vitamins) |
| Post‑delivery (lactation) | Maintain maternal stores, enrich breast milk | 500 µg DFE |
Assessing Folate Status
- Serum folate test – Quick snapshot; useful after a recent dietary change or supplement initiation.
- RBC folate test – Gold standard for chronic adequacy; especially important in preconception evaluation.
- Homocysteine level – Elevated homocysteine can signal functional folate deficiency (often alongside B12 deficiency).
Interpretation tip: An isolated low serum folate with normal RBC folate usually indicates a temporary dip (e.g., after fasting). Conversely, low RBC folate confirms a true depletion requiring intervention.
Strategies to Optimize Folate Status
Dietary Approaches
- Eat a “rainbow” of vegetables: Aim for at least 2–3 servings of dark leafy greens daily.
- Incorporate legumes: Replace meat portions 2–3 times per week with lentils or chickpeas.
- Choose fortified grains: Opt for whole‑grain breads, cereals, and pasta that list “folic acid added.”
- Limit cooking losses: Steam vegetables for 3–5 minutes; avoid boiling large volumes of water that are later discarded.
Supplementation Guidelines
| Situation | Recommended Form | Dose | Frequency |
|---|---|---|---|
| General adult (no special risk) | Folic acid (synthetic) | 400 µg DFE (≈ 600 µg folic acid) | Once daily |
| Women planning pregnancy | Folic acid | 400–800 µg DFE | Once daily, start ≥ 1 mo before conception |
| MTHFR C677T homozygous or malabsorption | 5‑MTHF (active) | 400–800 µg DFE | Once daily |
| On methotrexate or antiepileptic meds | 5‑MTHF + B12 | 800–1 000 µg DFE | Split dose (morning/evening) |
| Elderly with renal impairment | Folic acid (lower dose) | 200–400 µg DFE | Once daily |
Safety note: Exceeding the UL (1 000 µg synthetic folic acid per day) can mask vitamin B12 deficiency, potentially leading to irreversible neurologic damage. Supplemental 5‑MTHF does not have the same masking effect and may be preferable for high‑dose regimens.
Lifestyle Enhancements
- Reduce alcohol intake: Even moderate consumption (≥ 2 drinks/day) reduces folate absorption.
- Quit smoking: Tobacco oxidizes folate and increases urinary loss.
- Manage chronic conditions: Optimizing diabetes control and treating gastrointestinal disorders improves folate utilization.
Potential Risks of Inadequate or Excess Folate
| Condition | Folate Status | Clinical Manifestations |
|---|---|---|
| Deficiency | Serum < 3 ng/mL or RBC < 140 ng/mL | Megaloblastic anemia, glossitis, fatigue, neuropsychiatric changes, increased risk of neural‑tube defects in offspring |
| Over‑supplementation (synthetic folic acid > 1 mg/day) | High serum folate, normal RBC | May mask B12 deficiency, potentially precipitating neuropathy; theoretical increased risk of certain cancers (data inconclusive) |
| Unmetabolized folic acid | Elevated plasma folic acid after high‑dose supplements | Possible alteration of immune function; clinical relevance still under investigation |
Bottom line: Aim for adequate intake, not excessive. Regular monitoring is essential for high‑risk individuals.
Practical Action Plan
- Screen: If you are planning pregnancy, request a CBC and RBC folate test.
- Diet: Add at least two servings of folate‑rich vegetables and one legume serving daily.
- Supplement: Begin a prenatal vitamin containing 400–800 µg DFE of folic acid at least 30 days before conception.
- Monitor: Re‑check serum folate after 4–6 weeks of supplementation; if still low, consider increasing dose or switching to 5‑MTHF.
- Lifestyle: Limit alcohol, quit smoking, and manage chronic illnesses to enhance folate metabolism.
Frequently Asked Questions
What is the most common cause of abnormal Folate (Vitamin B9) levels?
The leading cause of low folate is inadequate dietary intake, often compounded by chronic alcohol consumption, malabsorptive gastrointestinal disorders (e.g., celiac disease), or the use of medications that interfere with folate metabolism such as antiepileptics and methotrexate. In contrast, elevated serum folate usually results from excessive intake of synthetic folic acid through fortified foods or high‑dose supplements, especially when the liver’s capacity to convert folic acid to its active form is exceeded.
How often should I get my Folate (Vitamin B9) tested?
For the general adult population, a once‑every‑2‑3 years screening is sufficient if dietary habits are stable and there are no risk factors. Women who are planning pregnancy, pregnant women, or individuals on folate‑interfering medications should have their serum folate evaluated before conception and then every trimester during pregnancy. Patients with known malabsorption syndromes or genetic polymorphisms affecting folate metabolism may require quarterly monitoring while adjusting supplementation.
Can lifestyle changes improve my Folate (Vitamin B9) levels?
Absolutely. Increasing consumption of folate‑rich foods (leafy greens, legumes, fortified grains) directly raises intake. Reducing alcohol intake and quitting smoking improve intestinal absorption and decrease urinary loss. Managing chronic illnesses such as diabetes and inflammatory bowel disease, and reviewing medication regimens with a healthcare provider, can also enhance folate status. Combining these lifestyle modifications with appropriate supplementation often normalizes folate levels more rapidly than diet alone.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.