Normal Vitamin E Ranges and Interpretation
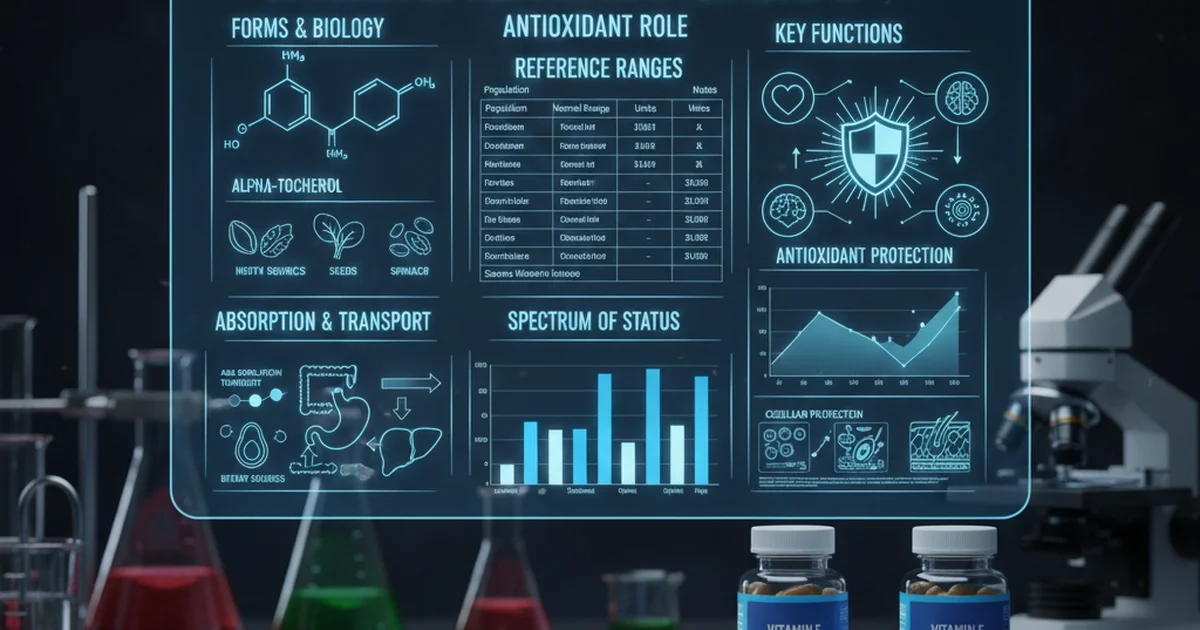
Vitamin E is a group of eight fat-soluble compounds, encompassing four tocopherols (alpha, beta, gamma, delta) and four tocotrienols (alpha, beta, gamma, delta). Of these, alpha-tocopherol is the only form recognized to meet human requirements and is the most biologically active form found in the human body. As a potent antioxidant, Vitamin E plays a crucial role in protecting cells from oxidative damage caused by free radicals, which are byproducts of normal metabolism and environmental stressors. Understanding normal Vitamin E ranges, its dietary sources, bioavailability, and the implications of supplementation is essential for maintaining optimal health.
Understanding Vitamin E: A Vital Nutrient
Vitamin E's primary function is its antioxidant activity. It works by neutralizing free radicals, thereby preventing damage to cell membranes, lipoproteins, and DNA. This protective role has far-reaching implications for various bodily systems:
- Cardiovascular Health: By preventing the oxidation of LDL ("bad") cholesterol, Vitamin E may help reduce the risk of atherosclerosis.
- Immune Function: It supports the immune system by enhancing the production of immune cells and improving resistance to infectious diseases.
- Eye Health: Vitamin E, along with other antioxidants, is thought to play a role in preventing age-related macular degeneration and cataracts.
- Skin Health: Its antioxidant properties contribute to skin protection against UV radiation and pollution, potentially supporting skin integrity and healing.
- Neurological Function: Vitamin E is concentrated in nerve tissues, and its antioxidant action is vital for maintaining neurological health, protecting against oxidative stress that can contribute to neurodegenerative diseases.
Given these critical functions, maintaining adequate Vitamin E levels is paramount for overall well-being.
Dietary Sources of Vitamin E
Unlike water-soluble vitamins, Vitamin E is stored in the body's fatty tissues, primarily the liver. Humans cannot synthesize Vitamin E, making it an essential nutrient that must be obtained through diet or supplementation.
Rich Food Sources
The best way to ensure sufficient Vitamin E intake is through a balanced diet rich in specific foods:
- Vegetable Oils: Wheat germ oil, sunflower oil, safflower oil, corn oil, and soybean oil are excellent sources. Olive oil contains moderate amounts.
- Nuts: Almonds, hazelnuts, peanuts, and pecans are particularly rich in Vitamin E.
- Seeds: Sunflower seeds are a powerhouse of Vitamin E.
- Green Leafy Vegetables: Spinach, kale, and broccoli contribute to Vitamin E intake, though in smaller amounts compared to oils and nuts.
- Fortified Foods: Some breakfast cereals, margarines, and fruit juices are fortified with Vitamin E.
- Other Sources: Avocado, asparagus, and certain seafood also provide Vitamin E.
Importance of Whole Foods
Obtaining Vitamin E from whole foods is generally preferred as it provides a complex matrix of nutrients, including other antioxidants and beneficial compounds that work synergistically. For instance, many plant-based sources offer a mix of tocopherols and tocotrienols, each with unique biological activities, although alpha-tocopherol is the primary form that the human body actively maintains.
Bioavailability and Metabolism
The journey of Vitamin E from food to cellular utilization is complex, involving digestion, absorption, transport, and selective retention.
Absorption and Transport
As a fat-soluble vitamin, Vitamin E's absorption is intimately linked to dietary fat intake:
- Digestion: In the stomach and small intestine, dietary fats are emulsified by bile acids and broken down by pancreatic enzymes. Vitamin E is released from the food matrix during this process.
- Absorption: Vitamin E is then absorbed into intestinal cells (enterocytes) along with other fats. This process requires the presence of bile salts and pancreatic enzymes. Conditions affecting fat absorption, such as cystic fibrosis, Crohn's disease, or celiac disease, can significantly impair Vitamin E uptake.
- Chylomicron Formation: Once inside the enterocytes, Vitamin E is incorporated into chylomicrons, which are lipoprotein particles that transport dietary fats through the lymphatic system into the bloodstream.
- Liver Processing: Chylomicrons deliver Vitamin E to the liver. The liver plays a critical role in metabolizing and distributing Vitamin E. It contains a specific protein called alpha-tocopherol transfer protein (α-TTP), which preferentially binds to alpha-tocopherol and incorporates it into very-low-density lipoproteins (VLDLs). This selective mechanism ensures that alpha-tocopherol is the predominant form of Vitamin E in human plasma and tissues. Other forms of Vitamin E (beta, gamma, delta tocopherols and tocotrienols) are less efficiently transferred and are largely metabolized and excreted.
- Circulation: VLDLs then circulate in the bloodstream, delivering alpha-tocopherol to various tissues. As VLDLs lose triglycerides, they become low-density lipoproteins (LDL) and high-density lipoproteins (HDL), which also carry Vitamin E. Therefore, plasma Vitamin E levels are highly correlated with plasma lipid concentrations.
Factors Affecting Bioavailability
Several factors can influence the bioavailability of Vitamin E:
- Dietary Fat Intake: Adequate fat intake is essential for optimal absorption. Very low-fat diets can lead to reduced Vitamin E absorption.
- Gastrointestinal Health: Any condition that impairs fat digestion or absorption will reduce Vitamin E bioavailability.
- Genetic Factors: Rare genetic disorders affecting α-TTP can lead to severe Vitamin E deficiency.
- Food Matrix: The form in which Vitamin E is present in food can affect its release and absorption.
Normal Vitamin E Ranges and Their Significance
Measuring Vitamin E levels, typically serum alpha-tocopherol, can be a valuable tool in assessing nutritional status, particularly in individuals with malabsorption disorders or those at risk of deficiency. [Understanding how these levels are measured] is key to interpreting the results accurately.
Factors Influencing Reference Ranges
It's important to note that Vitamin E reference ranges can vary between laboratories due to different analytical methods, equipment, and calibration standards. Furthermore, individual factors significantly influence these levels:
- Age: Infants and young children often have lower plasma Vitamin E levels due to lower fat stores and developing digestive systems.
- Lipid Levels: As Vitamin E is transported by lipoproteins, serum Vitamin E levels are directly correlated with total lipid levels (cholesterol and triglycerides). A seemingly low Vitamin E level might be normal in an individual with very low lipid levels, while a normal Vitamin E level could indicate relative deficiency in someone with hyperlipidemia. For precise assessment, Vitamin E levels are sometimes expressed as a ratio to total lipids or cholesterol (e.g., mg Vitamin E per gram of total lipids).
- Disease States: Conditions affecting fat absorption, liver function, or genetic disorders can impact levels.
Detailed Reference Ranges Table
Here is a general guide to normal serum alpha-tocopherol ranges. These ranges are approximate and may vary based on the specific laboratory and its methodologies. Always consult with a healthcare professional for personalized interpretation of your results.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 5000-20000 | ng/mL | Often correlated with total lipid levels |
| Adult Women | 5000-20000 | ng/mL | May be lower in women with very low lipid levels |
| Children (1-12 years) | 3000-15000 | ng/mL | Age-dependent, lower end for younger children |
| Infants (0-12 months) | 1000-8000 | ng/mL | Lower due to underdeveloped fat absorption, premature infants at higher risk of deficiency |
Interpretation of Normal Ranges
A result within the normal range generally indicates adequate Vitamin E status. However, it's crucial to consider the individual's overall health, dietary habits, and any underlying medical conditions. A "normal" level doesn't always guarantee optimal status, especially if there are symptoms suggestive of deficiency or if the individual has very high lipid levels.
Interpreting High Vitamin E Levels (Hypervitaminosis E)
While Vitamin E is essential, excessive intake, almost exclusively from high-dose supplementation, can lead to adverse effects. It is extremely rare to achieve toxic levels of Vitamin E from food sources alone.
Causes of High Levels
- Excessive Supplementation: The most common cause of hypervitaminosis E is the chronic intake of Vitamin E supplements far exceeding the recommended daily allowance (RDA) and the tolerable upper intake level (UL). The UL for adults is 1,000 mg (1,500 IU) of alpha-tocopherol per day from supplements.
Symptoms and Risks
The primary and most significant risk of excessive Vitamin E intake is an increased risk of bleeding. This occurs because high doses of Vitamin E can inhibit Vitamin K-dependent clotting factors, thereby interfering with blood coagulation.
Other potential risks and symptoms include:
- Increased risk of hemorrhagic stroke: Studies have suggested a potential link between very high doses of Vitamin E and an increased risk of certain types of stroke.
- Interaction with Anticoagulants: Individuals taking anticoagulant medications (blood thinners) such as warfarin are at a significantly higher risk of bleeding complications if they also take high doses of Vitamin E. This interaction can be life-threatening.
- Interference with Other Fat-Soluble Vitamins: High doses of Vitamin E may theoretically interfere with the absorption and utilization of other fat-soluble vitamins (A, D, K), although this is less commonly observed clinically compared to the bleeding risk.
- Mild Symptoms: Less severe symptoms can include nausea, diarrhea, stomach cramps, fatigue, and headache.
Due to these risks, individuals should not exceed the UL for Vitamin E without strict medical supervision.
Interpreting Low Vitamin E Levels (Vitamin E Deficiency)
Vitamin E deficiency is uncommon in healthy individuals with a balanced diet. When it does occur, it is usually due to underlying conditions that impair fat absorption or metabolism.
Causes of Low Levels
- Malabsorption Syndromes: This is the most common cause. Conditions like cystic fibrosis, chronic pancreatitis, cholestatic liver disease, Crohn's disease, celiac disease, and short bowel syndrome prevent the proper absorption of fats and, consequently, fat-soluble vitamins like Vitamin E.
- Genetic Disorders: Rare genetic disorders, such as abetalipoproteinemia and familial isolated Vitamin E deficiency (caused by mutations in the α-TTP gene), severely impair Vitamin E transport and utilization.
- Premature Infants: Premature and very low-birth-weight infants are at higher risk due to underdeveloped digestive systems and low fat stores.
- Very Low-Fat Diets: Extremely restrictive low-fat diets, especially if maintained long-term, can potentially lead to inadequate Vitamin E intake and absorption.
Symptoms and Risks
Vitamin E deficiency primarily affects the nervous system, leading to neurological symptoms. This is because nerve cells are particularly vulnerable to oxidative damage.
Key symptoms include:
- Neurological Impairment:
- Ataxia: Impaired coordination and balance.
- Peripheral neuropathy: Numbness, tingling, or weakness in the extremities.
- Muscle weakness (myopathy).
- Retinopathy: Damage to the retina of the eye, leading to vision problems.
- Slurred speech (dysarthria).
- Hemolytic Anemia: In infants, particularly premature ones, Vitamin E deficiency can lead to the premature destruction of red blood cells, causing anemia.
- Impaired Immune Response: Compromised immune function, increasing susceptibility to infections.
Untreated, severe Vitamin E deficiency can lead to irreversible neurological damage. Early diagnosis and intervention are crucial.
Supplementation Considerations
While a balanced diet is the cornerstone of adequate Vitamin E intake, supplementation may be necessary in specific circumstances.
When is Supplementation Necessary?
- Diagnosed Deficiency: Individuals with confirmed Vitamin E deficiency due to malabsorption disorders or genetic conditions almost always require supplementation, often at high doses under medical supervision.
- Certain Medical Conditions: In some cases, healthcare providers might recommend Vitamin E for specific conditions (e.g., certain neurological disorders, non-alcoholic fatty liver disease), though evidence for widespread benefits is often mixed.
- Premature Infants: Supplementation is often given to premature infants to prevent hemolytic anemia and other complications.
Forms of Vitamin E in Supplements
Vitamin E supplements come in various forms, which can be confusing:
- Natural Vitamin E (d-alpha-tocopherol): This form is derived from vegetable oils and is the most biologically active. It is often labeled as "natural" or "d-alpha-tocopherol."
- Synthetic Vitamin E (dl-alpha-tocopherol): This form is chemically synthesized and is less potent than natural Vitamin E. It is labeled as "dl-alpha-tocopherol." The body utilizes synthetic alpha-tocopherol about half as efficiently as natural alpha-tocopherol.
- Mixed Tocopherols: Some supplements provide a blend of alpha, beta, gamma, and delta tocopherols, which may offer broader antioxidant benefits, though alpha-tocopherol remains the primary form retained by the body.
- Tocotrienols: Less common in supplements, tocotrienols are another group of Vitamin E compounds found in palm oil, rice bran, and annatto. Research on their specific health benefits is ongoing.
For supplementation, natural alpha-tocopherol is generally preferred due to its higher bioavailability.
Dosage Recommendations and Upper Limits
The Recommended Dietary Allowance (RDA) for adults is 15 mg (22.4 IU) of alpha-tocopherol per day. This amount can typically be met through diet.
The Tolerable Upper Intake Level (UL) for adults from supplements is 1,000 mg (1,500 IU) of alpha-tocopherol per day. Exceeding this level significantly increases the risk of adverse effects, particularly bleeding.
Potential Interactions
- Anticoagulants (Blood Thinners): As mentioned, high doses of Vitamin E can interfere with Vitamin K and increase the risk of bleeding in individuals taking warfarin or other anticoagulants.
- Chemotherapy Drugs: There is some concern that high doses of antioxidants, including Vitamin E, might interfere with the effectiveness of certain chemotherapy drugs, although evidence is mixed. Patients undergoing cancer treatment should discuss all supplements with their oncologist.
- Statins: Some studies have suggested that high doses of antioxidant supplements, including Vitamin E, might blunt the beneficial effects of statins on cholesterol levels, though this finding is not consistently replicated.
Before starting any Vitamin E supplementation, especially at high doses, it is crucial to consult with a healthcare professional to assess individual needs and potential risks. This testing provides crucial data to guide such decisions, helping to determine if supplementation is truly warranted and at what dosage, while avoiding potential harm. [This testing provides crucial data] for making informed decisions about Vitamin E intake.
Actionable Advice for Maintaining Healthy Vitamin E Levels
Maintaining optimal Vitamin E levels is a proactive step towards long-term health.
- Prioritize Dietary Sources: Focus on a diet rich in nuts, seeds, vegetable oils (like sunflower or wheat germ oil), and green leafy vegetables. Incorporate avocados and fortified cereals.
- Ensure Adequate Fat Intake: Since Vitamin E is fat-soluble, consuming healthy fats with your meals will enhance its absorption. Think olive oil on salads or nuts as a snack.
- Address Malabsorption Issues: If you have a condition known to impair fat absorption, work closely with your healthcare provider to manage the underlying disease and monitor your Vitamin E status. Supplementation will likely be necessary.
- Be Cautious with Supplements: Do not exceed the Tolerable Upper Intake Level (UL) of 1,000 mg (1,500 IU) per day without medical guidance. Higher doses are rarely needed and carry significant risks, particularly if you are on blood-thinning medication.
- Regular Health Check-ups: If you are at risk for deficiency or considering supplementation, discuss Vitamin E testing with your doctor. They can interpret your results in the context of your overall health and medical history.
Conclusion
Vitamin E is an indispensable nutrient, primarily recognized for its powerful antioxidant capabilities that protect cellular integrity and support numerous physiological functions. While dietary sources are typically sufficient for most healthy individuals, understanding normal Vitamin E ranges, factors influencing its absorption and metabolism, and the implications of both deficiency and excess are vital. For those with malabsorption issues or specific medical conditions, targeted supplementation under medical supervision may be necessary. Always prioritize whole-food sources and consult a healthcare professional for personalized advice regarding Vitamin E intake and testing.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin E levels?
The most common cause of abnormally low Vitamin E levels is malabsorption syndromes, where the body struggles to absorb fats (and thus fat-soluble vitamins) from the digestive tract. Conditions like cystic fibrosis, Crohn's disease, celiac disease, chronic pancreatitis, and certain liver diseases fall into this category. Abnormally high Vitamin E levels are almost exclusively caused by excessive intake of Vitamin E supplements, far exceeding the recommended daily allowances and tolerable upper intake levels.
How often should I get my Vitamin E tested?
For most healthy individuals with a balanced diet and no symptoms of deficiency or malabsorption, routine Vitamin E testing is generally not necessary. However, testing may be recommended for:
- Individuals with conditions known to cause fat malabsorption.
- Those experiencing neurological symptoms consistent with Vitamin E deficiency.
- Premature infants or individuals with specific genetic disorders affecting Vitamin E metabolism.
- People taking high doses of Vitamin E supplements, especially if on anticoagulant medications, to monitor for potential adverse effects. The frequency of testing will depend on the individual's specific medical condition and the advice of their healthcare provider.
Can lifestyle changes improve my Vitamin E levels?
Yes, lifestyle changes, primarily dietary modifications, can significantly improve Vitamin E levels for most people. Focusing on a diet rich in Vitamin E sources such as nuts (almonds, hazelnuts), seeds (sunflower seeds), vegetable oils (wheat germ, sunflower, safflower), avocados, and green leafy vegetables (spinach, kale) is the most effective approach. Ensuring adequate, but not excessive, dietary fat intake will also enhance Vitamin E absorption. For individuals with underlying medical conditions causing malabsorption, addressing those conditions medically is paramount, alongside dietary strategies, and often requires targeted supplementation under professional guidance.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.