Vitamin E Test: Measuring Tocopherol Levels
Vitamin E is a fat-soluble nutrient essential for human health, primarily recognized for its potent antioxidant properties. It plays a crucial role in protecting cell membranes from oxidative damage caused by free radicals, which are unstable molecules that can harm cells. Beyond its antioxidant function, Vitamin E is involved in immune function, cell signaling, gene expression, and platelet aggregation.
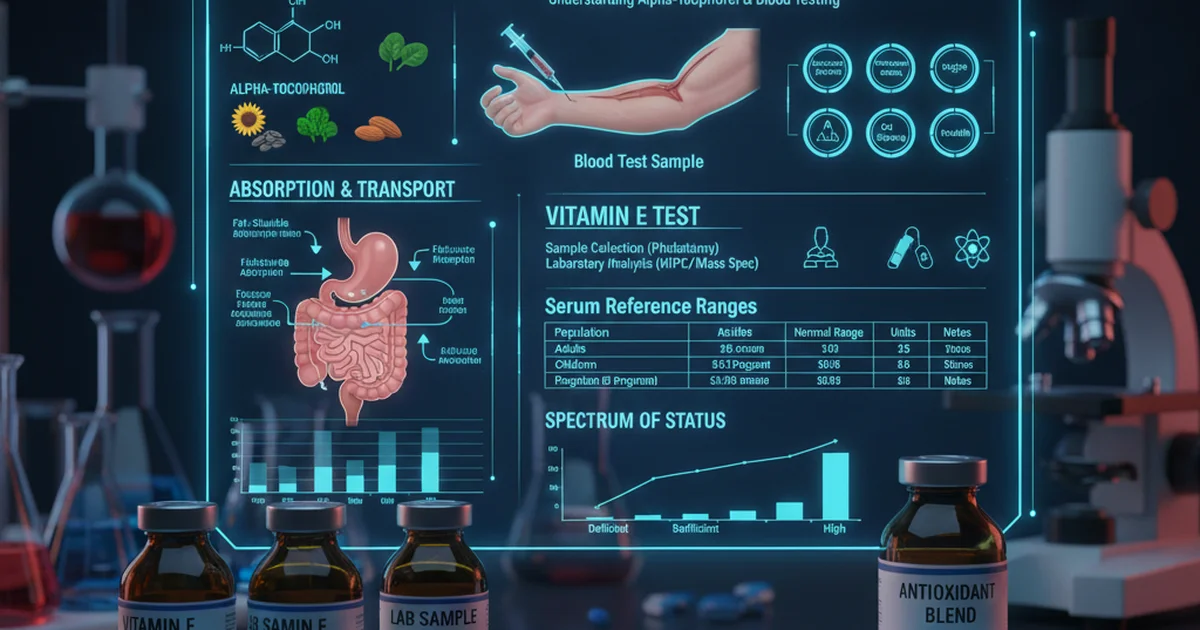
The term "Vitamin E" is a collective name for a group of eight fat-soluble compounds: four tocopherols (alpha, beta, gamma, and delta) and four tocotrienols (alpha, beta, gamma, and delta). Among these, alpha-tocopherol is the most biologically active form in humans and is the primary form measured in blood tests. When a "Vitamin E test" is performed, it typically quantifies the level of alpha-tocopherol in the blood serum or plasma.
Understanding the Vitamin E Test
A Vitamin E test involves a simple blood draw, usually from a vein in your arm. The blood sample is then sent to a laboratory to measure the concentration of tocopherols, predominantly alpha-tocopherol.
Why is the Test Performed?
Measuring Vitamin E levels is not a routine screening test for most healthy individuals. It is typically ordered when there is a suspicion of deficiency or malabsorption, or to monitor supplementation in specific clinical contexts. Reasons for testing may include:
- Symptoms of Deficiency: Patients presenting with neurological symptoms such as muscle weakness, gait disturbances (ataxia), visual problems (retinopathy), or impaired immune response, which are characteristic signs of severe Vitamin E deficiency.
- Malabsorption Syndromes: Conditions that impair fat absorption, such as cystic fibrosis, celiac disease, Crohn's disease, chronic pancreatitis, cholestatic liver disease, or short bowel syndrome, can lead to Vitamin E deficiency because it is a fat-soluble vitamin.
- Genetic Disorders: Rare genetic disorders, such as abetalipoproteinemia or familial isolated Vitamin E deficiency (ataxia with Vitamin E deficiency, AVED), can severely impair Vitamin E absorption or transport.
- Monitoring Supplementation: In individuals receiving high-dose Vitamin E supplementation for various conditions, testing may be done to ensure therapeutic levels are achieved or to prevent excessive accumulation.
- Premature Infants: Premature and low-birth-weight infants are at increased risk of Vitamin E deficiency due to immature digestive and liver systems.
What Does the Test Measure?
The test primarily measures serum or plasma alpha-tocopherol concentration. Because Vitamin E is transported in the blood by lipoproteins (fat-carrying proteins), its concentration is highly correlated with total serum lipid levels. Therefore, interpreting Vitamin E levels often requires considering the patient's lipid profile (e.g., total cholesterol and triglycerides). In some cases, a Vitamin E:Total Lipid Ratio is calculated to provide a more accurate assessment, especially in individuals with abnormal lipid profiles.
Reference Ranges for Vitamin E (Alpha-Tocopherol)
Interpreting Vitamin E levels requires understanding the typical reference ranges, which can vary slightly between laboratories and are often influenced by factors like age and lipid status. The following table provides general reference ranges for total alpha-tocopherol in serum or plasma.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adults (General) | 5-20 | mg/L | Often corrected for total lipids; 0.8 mg/g total lipids is a common threshold |
| Children (1-12 years) | 3-12 | mg/L | Age-dependent; lower ranges in younger children, also lipid-corrected |
| Deficiency Threshold | < 5 | mg/L | Generally considered deficient if uncorrected, or < 0.5 mg/g total lipids |
| Toxicity Concerns | > 30 | mg/L | Levels above this, especially with supplementation, may warrant investigation |
Note on Units: Vitamin E levels are most commonly reported in milligrams per liter (mg/L) or micromoles per liter (µmol/L). Some laboratories may report in micrograms per deciliter (µg/dL), where 1 mg/L equals 100 µg/dL. The ranges provided are for total alpha-tocopherol in serum or plasma.
Interpreting High Vitamin E Levels
While Vitamin E is generally considered safe, excessively high levels, usually due to high-dose supplementation, can pose risks.
- Symptoms of Toxicity: Symptoms are rare but can include increased bleeding risk (due to interference with Vitamin K metabolism), nausea, diarrhea, stomach cramps, fatigue, and muscle weakness.
- Increased Bleeding Risk: This is the most significant concern with high-dose Vitamin E supplementation, especially in individuals taking anticoagulant medications (blood thinners) like warfarin or antiplatelet drugs. High doses can inhibit platelet aggregation and interfere with Vitamin K-dependent clotting factors, increasing the risk of hemorrhage.
- Interference with Other Nutrients: Very high doses of Vitamin E can potentially interfere with the absorption and utilization of other fat-soluble vitamins, particularly Vitamin K.
- Sources of High Levels: Almost always attributed to excessive intake from supplements, as dietary intake alone is highly unlikely to lead to toxic levels.
Interpreting Low Vitamin E Levels
Low Vitamin E levels, or deficiency, are less common in healthy individuals with adequate diets but can have significant health consequences.
- Symptoms of Deficiency:
- Neurological Impairment: The most prominent symptoms are neurological, including peripheral neuropathy (nerve damage leading to numbness, tingling, and weakness), ataxia (loss of coordination and balance), myopathy (muscle weakness), and retinopathy (damage to the retina of the eye). These symptoms arise because nerve cells are particularly vulnerable to oxidative damage, and Vitamin E protects cell membranes.
- Impaired Immune Response: Deficiency can weaken the immune system, making individuals more susceptible to infections.
- Hemolytic Anemia: In severe cases, especially in premature infants, Vitamin E deficiency can lead to the breakdown of red blood cells (hemolysis) due to increased oxidative stress on their membranes.
- Risk Factors for Deficiency:
- Malabsorption Syndromes: As mentioned, conditions affecting fat absorption are primary causes.
- Genetic Disorders: Abetalipoproteinemia and AVED.
- Premature Infants: Due to low fat stores, immature gastrointestinal tracts, and rapid growth.
- Chronic Diseases: Liver disease, gallbladder disease, and pancreatic insufficiency can impair Vitamin E absorption and transport.
- Very Low-Fat Diets: While rare, extremely restrictive very-low-fat diets over extended periods could theoretically contribute to deficiency.
Dietary Sources of Vitamin E
The best way to obtain Vitamin E is through a balanced diet rich in specific foods. Natural sources primarily provide alpha-tocopherol, but also other tocopherols and tocotrienols, which may have their own health benefits.
- Vegetable Oils: Wheat germ oil is an exceptionally rich source. Other significant sources include sunflower oil, safflower oil, corn oil, and soybean oil. Olive oil contains moderate amounts.
- Nuts and Seeds: Almonds, sunflower seeds, hazelnuts, and peanuts are excellent sources.
- Green Leafy Vegetables: Spinach, kale, collard greens, and Swiss chard contribute to Vitamin E intake.
- Avocado: A good source of Vitamin E and healthy fats.
- Fortified Foods: Some cereals, margarines, and juices are fortified with Vitamin E.
- Certain Fruits: Kiwi and mango contain modest amounts.
It is important to note that Vitamin E is sensitive to heat and light, so cooking methods and storage can affect its content in foods. Minimally processed foods and raw sources tend to retain more Vitamin E.
Bioavailability of Vitamin E
Bioavailability refers to the proportion of a nutrient that is absorbed from the diet and becomes available for use or storage in the body. For Vitamin E, this process is complex and involves several steps:
- Digestion and Release: Dietary Vitamin E, often esterified (bound to fatty acids) in foods, is released during digestion by pancreatic enzymes and bile salts in the small intestine.
- Micelle Formation: Once released, free tocopherols are incorporated into mixed micelles with other fats and bile salts. This micelle formation is crucial for their solubility and transport across the intestinal wall.
- Absorption: Micelles transport Vitamin E to the brush border of intestinal cells (enterocytes), where it is absorbed. Adequate dietary fat intake is essential for optimal absorption of Vitamin E, as it is a fat-soluble vitamin.
- Chylomicron Formation: Inside the enterocytes, Vitamin E is re-esterified and packaged into chylomicrons, which are lipoprotein particles responsible for transporting dietary fats from the intestine into the lymphatic system and then into the bloodstream.
- Liver Uptake and Redistribution: Chylomicrons deliver Vitamin E to various tissues, including the liver. The liver plays a critical role in metabolizing and redistributing Vitamin E. It selectively incorporates alpha-tocopherol into very-low-density lipoproteins (VLDLs) for transport to peripheral tissues, largely due to the action of the alpha-tocopherol transfer protein (α-TTP). This protein is why alpha-tocopherol is the predominant form in human plasma and tissues, even if other forms are abundant in the diet. The other forms of tocopherols and tocotrienols are generally metabolized and excreted more rapidly.
- Cellular Uptake: VLDLs are converted to low-density lipoproteins (LDLs) and then taken up by cells throughout the body via LDL receptors, delivering Vitamin E to cell membranes, where it exerts its antioxidant effects.
Factors influencing bioavailability:
- Dietary Fat Intake: Insufficient fat in a meal can significantly reduce Vitamin E absorption.
- Pancreatic and Biliary Function: Impaired production or flow of pancreatic enzymes or bile salts (e.g., in cystic fibrosis, cholestasis) severely limits Vitamin E absorption.
- Genetic Factors: Mutations in the α-TTP gene can lead to familial isolated Vitamin E deficiency (AVED), despite normal dietary intake and absorption, because the liver cannot effectively incorporate alpha-tocopherol into VLDLs for systemic distribution.
- Other Nutrients: High doses of other fat-soluble vitamins (A, D, K) or certain minerals might theoretically compete for absorption, though this is less common with typical dietary intake.
Supplementation of Vitamin E
Vitamin E supplementation is often considered for individuals with confirmed deficiency, malabsorption issues, or specific medical conditions. However, routine supplementation for the general healthy population without medical indication is generally not recommended and can carry risks, especially at high doses.
Forms of Vitamin E in Supplements
Supplements typically contain alpha-tocopherol in two main forms:
- Natural Vitamin E (d-alpha-tocopherol): Derived from vegetable oils, this is the naturally occurring form and is considered more bioavailable than synthetic forms. It is often labeled as "d-alpha-tocopherol," "RRR-alpha-tocopherol," or "natural Vitamin E."
- Synthetic Vitamin E (dl-alpha-tocopherol): Produced chemically, this is a mixture of eight stereoisomers, only one of which (RRR-alpha-tocopherol) is identical to natural alpha-tocopherol. It is labeled as "dl-alpha-tocopherol" or "synthetic Vitamin E." The bioavailability of synthetic alpha-tocopherol is approximately half that of natural alpha-tocopherol.
Many supplements also contain mixed tocopherols or tocotrienols, which provide the other forms of Vitamin E. While these may have unique benefits, alpha-tocopherol is still the primary form for which a Recommended Dietary Allowance (RDA) is established.
Recommended Dietary Allowance (RDA) and Tolerable Upper Intake Level (UL)
- RDA for Adults: 15 mg (or 22.4 IU of natural Vitamin E; 33.3 IU of synthetic Vitamin E) of alpha-tocopherol per day.
- Tolerable Upper Intake Level (UL) for Adults: 1,000 mg (or 1,500 IU of natural Vitamin E; 1,100 IU of synthetic Vitamin E) of alpha-tocopherol per day. Exceeding the UL significantly increases the risk of adverse effects, particularly bleeding.
When is Supplementation Indicated?
- Confirmed Deficiency: Individuals with documented low Vitamin E levels, especially those with neurological symptoms.
- Malabsorption Syndromes: Patients with conditions like cystic fibrosis, Crohn's disease, or chronic pancreatitis often require lifelong Vitamin E supplementation. Doses are typically much higher than the RDA and should be monitored by a healthcare professional.
- Genetic Disorders: Patients with abetalipoproteinemia or AVED require very high doses of alpha-tocopherol to overcome impaired transport mechanisms and prevent severe neurological degeneration.
- Premature Infants: May receive Vitamin E supplementation to prevent hemolytic anemia and other complications, under strict medical supervision.
Risks and Precautions with Supplementation
- Bleeding Risk: This is the most critical concern. High doses of Vitamin E can interfere with blood clotting and increase the risk of hemorrhage, especially in individuals on anticoagulants (e.g., warfarin), antiplatelet drugs (e.g., aspirin, clopidogrel), or those undergoing surgery. Patients should always inform their doctor about Vitamin E supplementation, especially before any surgical procedure.
- Interaction with Medications: Besides anticoagulants, Vitamin E may interact with other medications, including chemotherapy drugs (though evidence is mixed) and lipid-lowering drugs (statins), potentially reducing their effectiveness.
- Increased Mortality Risk: Some large-scale studies have suggested a slight increase in all-cause mortality with very high-dose Vitamin E supplementation (e.g., >400 IU/day) in certain populations, although these findings are debated and not universally accepted.
- Prostate Cancer Risk: A large clinical trial (SELECT) found that high-dose Vitamin E supplementation (400 IU/day of synthetic alpha-tocopherol) actually increased the risk of prostate cancer in healthy men. This underscores the importance of avoiding high-dose supplementation without a clear medical indication.
Actionable Advice for Maintaining Healthy Vitamin E Levels
- Prioritize Dietary Sources: The safest and most effective way to ensure adequate Vitamin E intake is through a diet rich in fruits, vegetables, nuts, seeds, and healthy oils. Focus on whole, unprocessed foods.
- Include Healthy Fats: Since Vitamin E is fat-soluble, consuming it with a source of healthy fats (e.g., avocado, nuts, olive oil) enhances its absorption.
- Be Mindful of Cooking: Minimize prolonged high-heat cooking of Vitamin E-rich oils, as heat can degrade the vitamin.
- Avoid Unnecessary High-Dose Supplements: Unless medically indicated and supervised by a healthcare professional, avoid taking Vitamin E supplements exceeding the RDA. There is no strong evidence for benefit in healthy individuals, and potential risks exist.
- Discuss with Your Doctor: If you have a medical condition affecting fat absorption, are taking medications, or are considering Vitamin E supplementation, always consult your physician or a registered dietitian. They can assess your individual needs, recommend appropriate testing, and guide safe and effective strategies.
- Monitor Symptoms: If you experience any neurological symptoms (muscle weakness, coordination issues, vision problems), seek medical attention. These could be signs of Vitamin E deficiency or other underlying conditions.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin E levels?
The most common cause of abnormally low Vitamin E levels is malabsorption of fats, which can stem from various gastrointestinal or liver disorders. Conditions like cystic fibrosis, celiac disease, Crohn's disease, chronic pancreatitis, cholestatic liver disease, or short bowel syndrome impair the body's ability to absorb dietary fats, and since Vitamin E is fat-soluble, its absorption is similarly compromised. Rare genetic disorders like abetalipoproteinemia or ataxia with Vitamin E deficiency (AVED) can also cause very low levels. Conversely, the most common cause of abnormally high Vitamin E levels is excessive intake from high-dose dietary supplements, as it is highly unlikely to achieve toxic levels through food alone.
How often should I get my Vitamin E tested?
For most healthy individuals, routine Vitamin E testing is not recommended and is generally unnecessary. Testing is typically reserved for specific clinical situations where there is a suspicion of deficiency or malabsorption. This includes individuals presenting with unexplained neurological symptoms (such as muscle weakness, ataxia, or vision problems), those diagnosed with conditions known to cause fat malabsorption (e.g., cystic fibrosis, chronic pancreatitis, cholestatic liver disease), or premature infants. If you are taking high-dose Vitamin E supplements under medical supervision for a specific condition, your doctor may recommend periodic testing to monitor levels and ensure safety. The frequency of testing in these cases would be determined by your healthcare provider based on your individual health status and treatment plan.
Can lifestyle changes improve my Vitamin E levels?
Yes, lifestyle changes, primarily dietary modifications, can significantly improve and maintain healthy Vitamin E levels for most people.
- Increase Intake of Vitamin E-Rich Foods: Incorporating more vegetable oils (like wheat germ, sunflower, safflower), nuts (almonds, hazelnuts), seeds (sunflower seeds), avocados, and green leafy vegetables (spinach, kale) into your diet will naturally boost your intake of alpha-tocopherol.
- Ensure Adequate Healthy Fat Intake: Since Vitamin E is fat-soluble, consuming it alongside healthy fats (e.g., adding avocado to a salad, using olive oil in cooking) enhances its absorption. Restrictive very-low-fat diets can impair Vitamin E absorption.
- Minimize Processing of Oils: Choose minimally processed oils and store them in cool, dark places to preserve their Vitamin E content, as it is sensitive to heat and light.
- Address Underlying Medical Conditions: If low Vitamin E levels are due to a medical condition causing malabsorption, working with your doctor to manage that condition is a crucial lifestyle and medical intervention. While diet helps, these conditions often require specific medical treatments or targeted supplementation.
For individuals without underlying medical conditions affecting absorption, a balanced diet rich in whole foods is generally sufficient to maintain optimal Vitamin E levels.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.