High Vitamin E: Bleeding Risks and Toxicity
Vitamin E, a fat-soluble vitamin, is renowned for its powerful antioxidant properties, playing a crucial role in protecting cells from oxidative damage. While essential for health, the adage "more is not always better" holds particularly true for this nutrient. High doses of Vitamin E, especially from supplements, can lead to significant health risks, including an increased propensity for bleeding and other forms of toxicity. Understanding the delicate balance between beneficial intake and harmful excess is paramount for maintaining optimal health.
This comprehensive guide delves into the various facets of Vitamin E, from its natural dietary sources and how our bodies absorb it, to the specific dangers associated with high supplementation. We will explore the mechanisms behind its anticoagulant effects, identify populations at risk, and provide actionable advice on preventing toxicity.
Understanding Vitamin E: A Vital Antioxidant
Vitamin E is not a single compound but a group of eight fat-soluble compounds: four tocopherols (alpha, beta, gamma, and delta) and four tocotrienols (alpha, beta, gamma, and delta). Of these, alpha-tocopherol is the most biologically active form in humans and is the primary form found in supplements and fortified foods.
Its fundamental role in the body is that of an antioxidant, neutralizing harmful free radicals that can damage cell membranes, proteins, and DNA. This protective action is vital for maintaining cellular integrity and function throughout the body. Beyond its antioxidant prowess, Vitamin E also contributes to:
- Immune function: Supporting the body's defenses against pathogens.
- Cell signaling: Playing a role in communication pathways between cells.
- Gene expression: Influencing the activity of certain genes.
- Blood vessel health: Contributing to the dilation of blood vessels and preventing blood clot formation.
Given these critical functions, adequate Vitamin E intake is undoubtedly important. However, the benefits derived from moderate, dietary intake differ significantly from the potential risks associated with excessive supplementation.
Dietary Sources and Bioavailability
Nature provides abundant sources of Vitamin E, primarily in plant-based foods. Incorporating these into your daily diet is the safest and most effective way to ensure sufficient intake without the risks of toxicity.
Rich Dietary Sources:
- Vegetable Oils: Wheat germ oil, sunflower oil, safflower oil, corn oil, and soybean oil are particularly rich sources.
- Nuts: Almonds, peanuts, hazelnuts, and walnuts.
- Seeds: Sunflower seeds.
- Green Leafy Vegetables: Spinach, kale, and broccoli.
- Fortified Foods: Cereals, margarines, and some juices are often fortified with Vitamin E.
Bioavailability and Absorption:
Vitamin E, being fat-soluble, requires dietary fat for proper absorption in the digestive tract. It is absorbed in the small intestine, transported via chylomicrons into the lymphatic system, and eventually enters the bloodstream. From there, it is delivered to the liver and then distributed to various tissues.
The bioavailability of Vitamin E can vary depending on its source:
- Natural Vitamin E (RRR-alpha-tocopherol): Found in foods and some supplements, this form is generally considered more bioavailable and potent than its synthetic counterpart.
- Synthetic Vitamin E (all-rac-alpha-tocopherol): Commonly found in fortified foods and many supplements, it is about half as potent as natural Vitamin E. The body preferentially retains the natural form.
Factors like malabsorption disorders (e.g., cystic fibrosis, Crohn's disease, chronic pancreatitis) can impair Vitamin E absorption, potentially leading to [vitamin E deficiency, with rare signs and nervous system risks]. Conversely, an extremely high intake of Vitamin E, particularly from supplements, can overwhelm the body's metabolic pathways and lead to accumulation and adverse effects.
Vitamin E Supplementation: When and How?
Vitamin E supplements are widely available and often marketed for their antioxidant benefits, skin health, and anti-aging properties. While supplementation can be beneficial for certain individuals, it's crucial to approach it with caution and under medical guidance.
Reasons for Supplementation:
- Confirmed Deficiency: Individuals with malabsorption disorders or genetic conditions that impair Vitamin E metabolism may require supplementation.
- Specific Medical Conditions: In some cases, healthcare providers might recommend Vitamin E for specific conditions, though the evidence for many uses is debated.
Dosage Considerations:
The Recommended Dietary Allowance (RDA) for Vitamin E for adults is 15 mg (22.4 IU) of alpha-tocopherol daily. Many supplements, however, contain significantly higher doses, often hundreds or even thousands of milligrams. It is these high doses that pose the greatest risk.
Before considering any Vitamin E supplement, it's advisable to assess your current intake and health status. A [vitamin E test] can measure the levels of tocopherol in your blood, providing valuable insight into your nutritional status and helping guide any potential supplementation decisions. This test helps determine if you are truly deficient or already have adequate levels, making informed choices about supplementation much easier and safer.
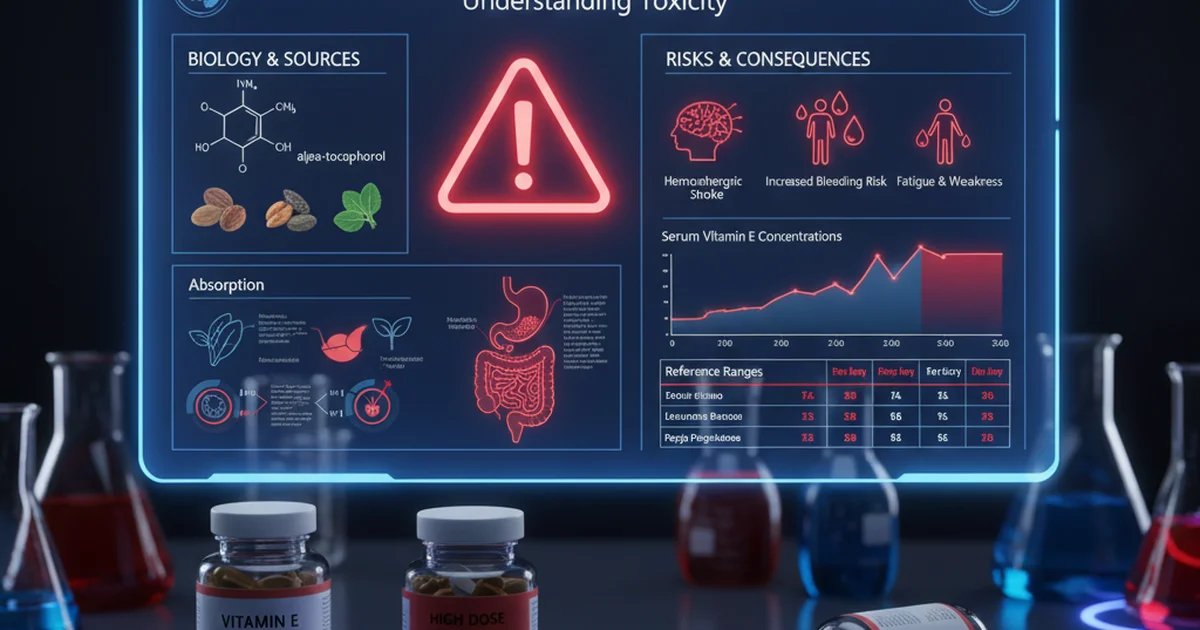
The Dangers of High Vitamin E: Bleeding Risks
One of the most significant and well-documented risks associated with high Vitamin E intake is its anticoagulant effect, which can increase the risk of bleeding. This is particularly concerning for individuals already on blood-thinning medications or those with underlying bleeding disorders.
Mechanism of Action:
Vitamin E's anticoagulant properties are primarily attributed to its interference with Vitamin K metabolism. Vitamin K is essential for the synthesis of several clotting factors in the liver. High doses of Vitamin E can inhibit the activity of Vitamin K-dependent carboxylase, an enzyme crucial for activating these clotting factors. By disrupting this pathway, Vitamin E can reduce the production of functional clotting factors, thereby prolonging clotting time and increasing the likelihood of bleeding.
Interaction with Anticoagulant Medications:
The interaction between high-dose Vitamin E and anticoagulant medications like warfarin (Coumadin) is particularly dangerous. Warfarin works by interfering with Vitamin K's action, and when combined with high Vitamin E, this effect is potentiated, leading to a synergistic increase in bleeding risk. Individuals taking these medications must exercise extreme caution and avoid high-dose Vitamin E supplements unless specifically advised and monitored by their physician. Other blood thinners, such as aspirin, clopidogrel, and newer oral anticoagulants, may also have their effects amplified by high Vitamin E intake.
Symptoms of Bleeding:
The signs of increased bleeding risk due to high Vitamin E can range from mild to severe:
- Easy bruising: Appearing without significant trauma.
- Nosebleeds: More frequent or prolonged.
- Bleeding gums: Especially during brushing.
- Heavy menstrual bleeding.
- Blood in urine or stool: Indicating internal bleeding.
- Prolonged bleeding from cuts.
- Petechiae or purpura: Small red or purple spots on the skin due to bleeding under the skin.
- Internal hemorrhages: In severe cases, high Vitamin E can contribute to life-threatening bleeding in the brain (hemorrhagic stroke) or other organs.
Any signs of unusual bleeding should prompt immediate medical attention, especially if you are taking Vitamin E supplements or blood thinners.
Toxicity and Other Adverse Effects
Beyond bleeding risks, excessively high doses of Vitamin E can lead to other forms of toxicity and adverse effects, though these are generally less severe than the bleeding complications.
Upper Limit (UL):
The Food and Nutrition Board of the Institute of Medicine has established a Tolerable Upper Intake Level (UL) for alpha-tocopherol from supplements and fortified foods. For adults aged 19 years and older, the UL is 1,000 mg (1,500 IU) per day. This limit is set to prevent the bleeding risks associated with high intake. It's important to note that this UL applies to alpha-tocopherol and does not typically include Vitamin E naturally present in foods, as toxicity from dietary sources alone is exceedingly rare.
Non-Bleeding Related Side Effects:
While severe toxicity is uncommon, doses exceeding the UL can sometimes cause:
- Gastrointestinal disturbances: Nausea, diarrhea, abdominal cramps.
- Fatigue or weakness.
- Headaches.
- Blurred vision.
These symptoms are usually mild and resolve upon discontinuing the supplement.
Potential Long-Term Risks:
Some studies have explored potential long-term risks associated with very high Vitamin E supplementation, though findings have been mixed and often context-dependent:
- Increased risk of hemorrhagic stroke: In certain populations, high Vitamin E intake has been linked to an elevated risk of bleeding in the brain.
- Increased risk of prostate cancer: A large clinical trial (SELECT study) found that high-dose Vitamin E supplementation (400 IU/day) slightly increased the risk of prostate cancer in healthy men, though this finding requires careful interpretation and further research.
- Interference with other fat-soluble vitamins: High doses of one fat-soluble vitamin can potentially interfere with the absorption or metabolism of others, such as Vitamins A and K.
Understanding and adhering to [normal vitamin E ranges and interpretation] is crucial for preventing these adverse effects. Regular monitoring, especially for individuals on long-term supplementation, can help ensure levels remain within a safe and beneficial window.
Identifying High Vitamin E Levels
Identifying high Vitamin E levels typically involves a combination of symptom recognition and diagnostic testing.
Symptoms of Toxicity:
As discussed, the most critical symptom to watch for is unusual bleeding. Other non-specific symptoms like nausea, diarrhea, fatigue, or headache can also be indicators, though they are less definitive.
Diagnostic Methods:
The most reliable way to confirm high Vitamin E levels is through a blood test that measures serum alpha-tocopherol concentrations. This test provides a quantitative measure of the Vitamin E circulating in your bloodstream. If you are concerned about your Vitamin E intake or experiencing symptoms, discussing a [vitamin E test measuring tocopherol levels] with your healthcare provider is the appropriate step.
When to Suspect High Levels:
You should suspect potentially high Vitamin E levels if:
- You are taking high-dose Vitamin E supplements, especially above the UL of 1,000 mg (1,500 IU) per day.
- You are experiencing unexplained bleeding, bruising, or other related symptoms.
- You are on anticoagulant medications and notice increased bleeding tendencies.
- You have been advised against high Vitamin E intake due to specific medical conditions.
Reference Ranges for Vitamin E
Understanding what constitutes a "normal" Vitamin E level is essential for interpreting test results. These ranges can vary slightly between laboratories and may be influenced by age, sex, and underlying health conditions. The following table provides general reference ranges for serum alpha-tocopherol:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 5,000-20,000 | ng/mL | Optimal levels may vary |
| Adult Women | 5,000-20,000 | ng/mL | Can be slightly lower in pregnancy |
| Children (1-12 yrs) | 3,000-10,000 | ng/mL | Age-dependent, consult pediatrician |
| Infants (0-1 yr) | 500-2,000 | ng/mL | Lower in premature infants |
Note: These ranges are for serum alpha-tocopherol, the most common form measured. Optimal levels are often considered to be in the mid-to-upper end of these ranges. Levels significantly above these ranges, especially when combined with high supplemental intake, warrant medical evaluation. For a more detailed understanding of what your specific test results mean, refer to an article on [normal vitamin E ranges and interpretation].
Managing High Vitamin E Levels
If high Vitamin E levels are identified or suspected, prompt action is necessary to mitigate risks.
Reducing Supplement Intake:
The most immediate and effective step is to discontinue or significantly reduce the dosage of Vitamin E supplements. This should always be done under the guidance of a healthcare professional, especially if you are on other medications or have underlying health conditions.
Dietary Adjustments:
While toxicity from dietary Vitamin E is rare, reviewing your diet to ensure you are not over-consuming fortified foods can be a complementary step, though usually not the primary cause of dangerously high levels. Focus on a balanced diet rich in various nutrients rather than excessive intake of any single food source.
Medical Supervision:
Close medical supervision is crucial, particularly for individuals with bleeding disorders, those on anticoagulant therapy, or those experiencing significant symptoms. Your doctor may monitor your blood clotting parameters (e.g., INR for warfarin users) and repeat Vitamin E level tests to ensure levels return to a safe range. In contrast to the rare but serious risks of excess, [vitamin E deficiency, though rare, has specific signs and nervous system risks] that also require careful medical management.
Actionable Advice and Prevention
Preventing Vitamin E toxicity involves a mindful approach to supplementation and a strong emphasis on dietary intake.
- Prioritize Dietary Sources: Aim to meet your Vitamin E needs through a diverse diet rich in nuts, seeds, vegetable oils, and green leafy vegetables. This approach provides Vitamin E in its natural matrix, alongside other beneficial nutrients, and poses virtually no risk of toxicity.
- Be Cautious with Supplements: If you choose to take Vitamin E supplements, opt for doses at or below the Recommended Dietary Allowance (RDA) of 15 mg (22.4 IU) per day, unless specifically advised otherwise by a healthcare professional. Avoid high-dose supplements (hundreds or thousands of IU) unless under strict medical supervision.
- Consult a Healthcare Professional: Always discuss any supplement regimen with your doctor, especially if you have existing health conditions, are pregnant or breastfeeding, or are taking other medications (particularly blood thinners). Your physician can help you determine if supplementation is necessary and at what dose.
- Regular Monitoring for At-Risk Individuals: If you are on long-term Vitamin E supplementation or have conditions that affect its metabolism, periodic blood tests to measure your Vitamin E levels can be beneficial. Your doctor can interpret these results in the context of your overall health.
- Understand Interactions: Be aware that Vitamin E can interact with other medications and supplements. For example, it can interfere with chemotherapy drugs and may reduce the effectiveness of statins in some cases. Always inform your healthcare providers about all supplements you are taking.
In summary, while Vitamin E is an indispensable nutrient, its benefits are best realized through a balanced diet. The allure of high-dose supplementation for enhanced health can inadvertently lead to serious risks, most notably an increased propensity for bleeding. Informed choices, guided by medical expertise, are key to harnessing the advantages of Vitamin E without succumbing to its potential harms.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin E levels?
The most common cause of abnormally low Vitamin E levels is malabsorption disorders, where the body struggles to absorb fats and fat-soluble vitamins due to conditions like cystic fibrosis, Crohn's disease, or chronic pancreatitis. Abnormally high Vitamin E levels are almost exclusively caused by excessive intake from dietary supplements, as obtaining toxic levels from food alone is extremely rare.
How often should I get my Vitamin E tested?
Most healthy individuals with a balanced diet do not need routine Vitamin E testing. However, testing may be recommended if you:
- Have symptoms of Vitamin E deficiency (e.g., neurological issues, muscle weakness).
- Have a malabsorption disorder.
- Are taking high-dose Vitamin E supplements.
- Are on anticoagulant medications and your doctor suspects an interaction.
- Are monitoring the effectiveness of treatment for a deficiency. Your healthcare provider will determine the appropriate frequency based on your individual health status and risk factors.
Can lifestyle changes improve my Vitamin E levels?
Yes, lifestyle changes can significantly improve Vitamin E levels, particularly if they are low due to dietary inadequacy or malabsorption.
- Dietary Enrichment: Increasing your intake of Vitamin E-rich foods (nuts, seeds, vegetable oils, leafy greens) is the most natural and effective way to boost levels.
- Healthy Fat Intake: Since Vitamin E is fat-soluble, consuming a moderate amount of healthy fats (e.g., avocados, olive oil) with your meals can enhance its absorption.
- Managing Underlying Conditions: For individuals with malabsorption, managing the primary digestive disorder (e.g., through dietary modifications, enzyme replacement therapy) can improve overall nutrient absorption, including Vitamin E.
- Avoiding Excessive Alcohol: Chronic alcohol abuse can impair nutrient absorption and liver function, indirectly affecting Vitamin E status. These lifestyle adjustments focus on enhancing natural absorption and intake, promoting healthy levels without the risks associated with excessive supplementation.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.