When Do Doctors Order a Vitamin A Test?
Vitamin A is a crucial fat-soluble vitamin, essential for numerous physiological processes, ranging from maintaining healthy vision and robust immune function to supporting cellular growth and differentiation. While often associated with carrots and eye health, its role extends far beyond. As a nutrition and supplement expert with deep medical knowledge, understanding when and why a doctor might order a Vitamin A test is critical for both clinicians and patients. This article will delve into the clinical indications for Vitamin A testing, explore its dietary sources, bioavailability, and the complexities of supplementation, providing comprehensive, evidence-based insights.
Understanding Vitamin A: Forms and Functions
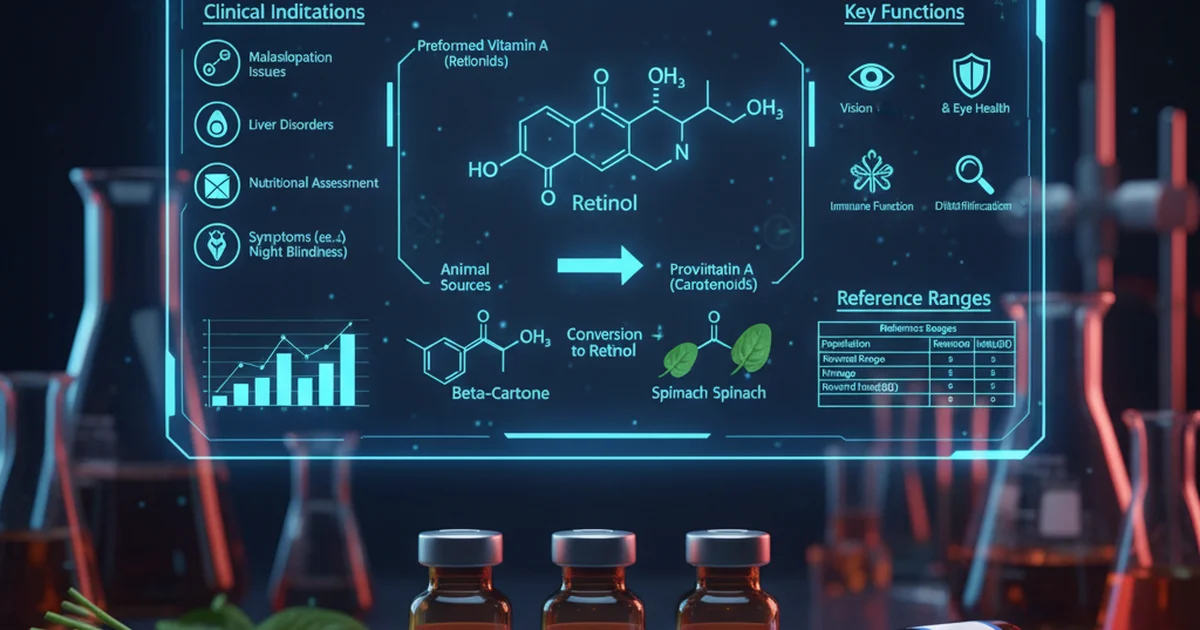
Vitamin A is a generic term for a group of fat-soluble compounds that are vital for human health. These compounds exist primarily in two forms:
- Preformed Vitamin A (Retinoids): Found in animal-sourced foods, this form includes retinol, retinal, and retinoic acid. Retinol is the most biologically active form and can be directly used by the body.
- Provitamin A Carotenoids: Found in plant-sourced foods, these include beta-carotene, alpha-carotene, and beta-cryptoxanthin. These compounds must be converted into retinol in the body, primarily in the small intestine and liver. Beta-carotene is the most efficient provitamin A carotenoid.
The body utilizes Vitamin A for a myriad of functions:
- Vision: Retinal is a key component of rhodopsin, a light-sensitive protein in the retina, crucial for low-light and color vision. Without adequate Vitamin A, the eyes cannot properly adapt to darkness, leading to night blindness. This is a primary reason why Vitamin A is so well-known for its [vitamin A benefits for vision and skin health].
- Immune Function: Vitamin A plays a vital role in the development and differentiation of various immune cells, including lymphocytes and phagocytes, supporting both innate and adaptive immunity.
- Cell Growth and Differentiation: Retinoic acid is essential for gene expression, influencing cell proliferation and differentiation, which is critical for the healthy development and maintenance of epithelial tissues, including skin, respiratory tract, and gut lining.
- Reproduction: It is involved in spermatogenesis and fetal development.
- Bone Health: Adequate Vitamin A is necessary for proper bone growth and remodeling.
Dietary Sources and Bioavailability
Maintaining optimal Vitamin A levels primarily relies on a balanced diet rich in both preformed Vitamin A and provitamin A carotenoids.
Preformed Vitamin A (Retinoids) Sources:
These sources provide retinol directly, making them highly bioavailable.
- Liver: Beef, chicken, and fish liver are exceptionally rich sources.
- Fish Oils: Cod liver oil is a potent source.
- Dairy Products: Milk, cheese, and butter (especially fortified varieties).
- Eggs: Egg yolks contain significant amounts.
Provitamin A Carotenoids Sources:
These plant-based sources require conversion in the body.
- Orange and Yellow Vegetables: Carrots, sweet potatoes, pumpkin, squash.
- Dark Green Leafy Vegetables: Spinach, kale, broccoli.
- Orange Fruits: Cantaloupe, apricots, mangoes.
Factors Affecting Bioavailability:
The bioavailability of Vitamin A, particularly from provitamin A carotenoids, can vary significantly.
- Fat Intake: Since Vitamin A is fat-soluble, dietary fat is crucial for its absorption. A meal lacking fat will lead to poor absorption of carotenoids.
- Food Matrix: Carotenoids are often tightly bound within plant matrices. Cooking and processing (e.g., pureeing carrots) can break down cell walls, increasing their release and absorption.
- Individual Conversion Efficiency: The conversion of carotenoids to retinol can vary widely among individuals due to genetic factors, nutritional status, and health conditions.
- Digestive Health: Conditions affecting fat digestion and absorption (e.g., pancreatic insufficiency, celiac disease, Crohn's disease) can impair Vitamin A uptake.
Why Doctors Order a Vitamin A Test: Clinical Indications
Doctors typically order a Vitamin A test, usually a serum retinol measurement, when there's a strong clinical suspicion of either deficiency or toxicity, or as part of a broader nutritional assessment in specific patient populations. It's not a routine screening test for healthy individuals.
Suspected Deficiency:
Vitamin A deficiency remains a significant public health problem globally, particularly in developing countries. In developed nations, it's more often associated with underlying medical conditions.
- Risk Factors for Deficiency:
- Malabsorption Syndromes: Conditions like cystic fibrosis, celiac disease, Crohn's disease, ulcerative colitis, chronic pancreatitis, and short bowel syndrome significantly impair fat absorption, thus hindering Vitamin A uptake.
- Chronic Liver Disease: The liver plays a central role in Vitamin A storage and metabolism. Liver diseases (e.g., cirrhosis, chronic hepatitis) can deplete stores.
- Bariatric Surgery: Gastric bypass and other malabsorptive bariatric procedures can lead to long-term nutrient deficiencies, including Vitamin A.
- Alcoholism: Chronic alcohol abuse can impair liver function and nutrient absorption.
- Severe Malnutrition: Inadequate dietary intake, often seen in eating disorders or poverty.
- Specific Medications: Certain medications, such as bile acid sequestrants, can interfere with fat-soluble vitamin absorption.
- Symptoms Suggesting Deficiency:
- Night Blindness (Nyctalopia): This is often the earliest and most common symptom, indicating impaired adaptation to low light.
- Xerophthalmia: A progressive eye disease ranging from conjunctival dryness (conjunctival xerosis) to corneal ulceration and potentially irreversible blindness.
- Bitot's Spots: Foamy, white, triangular patches on the conjunctiva.
- Impaired Immune Function: Recurrent infections, particularly respiratory and diarrheal illnesses.
- Follicular Hyperkeratosis (Phrynoderma): Dry, scaly skin with prominent hair follicles, often described as "toad skin."
- Poor Growth in Children: Especially in regions with endemic deficiency. For a more in-depth look at these indicators, you can refer to our article on [vitamin A normal range and deficiency signs].
Suspected Toxicity (Hypervitaminosis A):
While deficiency is a concern, excessive intake of preformed Vitamin A can be toxic. This is almost exclusively due to over-supplementation or consuming extremely large amounts of Vitamin A-rich foods (like polar bear liver), not from provitamin A carotenoids.
- Causes of Toxicity:
- Acute Toxicity: Ingestion of a single, very large dose of Vitamin A (e.g., >200,000 IU in adults).
- Chronic Toxicity: Regular intake of doses significantly above the Tolerable Upper Intake Level (UL) for prolonged periods (e.g., >100,000 IU/day for months). The UL for adults is 3,000 mcg RAE (10,000 IU) per day.
- Certain Medical Conditions: Individuals with impaired liver function or kidney disease may be more susceptible to Vitamin A accumulation and toxicity at lower doses.
- Symptoms Suggesting Toxicity:
- Acute Toxicity: Nausea, vomiting, headache, dizziness, blurred vision, muscle incoordination.
- Chronic Toxicity: Dry, rough skin, hair loss, cracked lips, fatigue, bone and joint pain, enlarged liver and spleen, elevated intracranial pressure (pseudotumor cerebri), and in severe cases, liver damage and coma. Understanding these symptoms is crucial, and further details can be found in our article on [hypervitaminosis A symptoms of vitamin A toxicity].
Monitoring Chronic Conditions:
For patients with conditions that predispose them to malabsorption or altered metabolism, regular Vitamin A testing may be part of their long-term management plan. This includes individuals with:
- Cystic fibrosis
- Chronic pancreatic insufficiency
- Celiac disease
- Inflammatory bowel disease
- Chronic liver disease
- Post-bariatric surgery patients
Pre- and Post-Surgery:
Especially before and after surgeries that affect the gastrointestinal tract, such as bariatric surgery or extensive bowel resections, Vitamin A levels may be assessed to establish a baseline and monitor for developing deficiencies.
Certain Dermatological Conditions:
Patients undergoing treatment with high-dose synthetic retinoids (e.g., isotretinoin for severe acne) may have their Vitamin A levels monitored, although these drugs are chemically distinct from Vitamin A, they can have similar systemic effects and interactions.
Nutritional Assessment in Vulnerable Populations:
In contexts of severe malnutrition, particularly in children or pregnant/lactating women in developing regions, Vitamin A testing helps guide public health interventions and individual treatment plans. However, due to practical limitations, clinical signs are often relied upon more heavily in such settings.
The Vitamin A Test: What It Measures
The most common method for assessing Vitamin A status is measuring serum retinol concentration.
- Serum Retinol: This test measures the amount of retinol circulating in the blood. It reflects recent dietary intake and liver stores to some extent.
- Limitations:
- Insensitivity to Early Deficiency: Serum retinol levels are tightly regulated by the liver. They often remain within the normal range until liver stores are severely depleted (i.e., less than 5% of normal), meaning a normal serum level does not rule out subclinical deficiency.
- Inflammation: During acute infections or inflammation (acute phase response), serum retinol levels can temporarily decrease, even if overall body stores are adequate, as retinol is sequestered in the liver. This can lead to a false impression of deficiency.
- Protein Status: Retinol circulates bound to retinol-binding protein (RBP). Protein-energy malnutrition can lead to low RBP levels, which in turn can lower serum retinol, even if liver stores of Vitamin A are sufficient.
Due to these limitations, clinical assessment, dietary history, and evaluation of underlying conditions are crucial for accurate interpretation of Vitamin A test results.
Interpreting Vitamin A Test Results
Interpreting Vitamin A test results requires careful consideration of the patient's clinical picture, risk factors, and symptoms. Results are typically categorized into deficient, normal, and potentially toxic ranges.
Detailed Reference Ranges Table
It's important to note that reference ranges can vary slightly between different laboratories. Always consult with your healthcare provider for the interpretation of your specific results.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 30-400 | ng/mL | Varies by lab, but this is a broad reference |
| Adult Women | 15-150 | ng/mL | Lower in premenopausal women due to physiological differences |
| Children | 7-140 | ng/mL | Highly age-dependent; lower in infants, increasing with age |
| Infants (0-6 months) | 10-20 | ng/mL | Generally lower, reflecting developmental stage |
Note on Units: Vitamin A levels can also be reported in µg/dL (micrograms per deciliter) or µmol/L (micromoles per liter). Conversion factors apply (1 ng/mL = 0.1 µg/dL; 1 µg/dL = 0.035 µmol/L). The most commonly reported unit for serum retinol in clinical settings is ng/mL or µg/dL.
- Deficient: Levels significantly below the lower end of the normal range indicate a deficiency. In adults, serum retinol levels <20 ng/mL (0.70 µmol/L) are generally considered deficient, while <10 ng/mL (0.35 µmol/L) indicates severe deficiency.
- Normal: Levels within the established reference range suggest adequate status.
- Potentially Toxic: Levels significantly above the upper end of the normal range, typically >200 ng/mL (7.0 µmol/L), especially if accompanied by symptoms, may indicate toxicity. Chronic levels >400 ng/mL (14 µmol/L) are often associated with hypervitaminosis A.
Supplementation and Safety Considerations
Vitamin A supplementation should always be approached with caution and ideally under medical supervision, especially for preformed Vitamin A.
- When Supplementation is Appropriate:
- Diagnosed Deficiency: When a Vitamin A deficiency is confirmed by testing and clinical signs, supplementation is necessary to restore levels and alleviate symptoms.
- High-Risk Individuals: Prophylactic supplementation may be considered in certain high-risk populations (e.g., children in endemic deficiency areas, post-bariatric surgery patients) as part of a comprehensive nutritional plan, but only with careful monitoring.
- Risks of Self-Supplementation:
- Toxicity: Over-the-counter Vitamin A supplements, particularly those containing preformed Vitamin A (retinyl palmitate or retinyl acetate), can easily lead to toxicity if taken in excessive doses. Unlike water-soluble vitamins, Vitamin A can accumulate in the body.
- Interactions: High doses of Vitamin A can interact with certain medications (e.g., blood thinners) and other nutrients.
- Pregnancy: Excessive Vitamin A intake during pregnancy (especially in the first trimester) is teratogenic and can cause birth defects. Pregnant women should avoid supplements containing more than 5,000 IU of preformed Vitamin A.
- Importance of Medical Guidance: A healthcare professional can accurately diagnose deficiency, determine the appropriate form and dosage of Vitamin A, and monitor for adverse effects. For provitamin A carotenoids like beta-carotene, the risk of toxicity is much lower as the body regulates its conversion to retinol. However, very high intakes of beta-carotene can cause a harmless yellowing of the skin (carotenodermia).
Actionable Advice for Maintaining Healthy Vitamin A Levels
For most healthy individuals, maintaining optimal Vitamin A levels can be achieved through dietary means.
- Embrace a Diverse, Balanced Diet:
- Regularly include a variety of orange, yellow, and dark green leafy vegetables and fruits (carrots, sweet potatoes, spinach, kale, mangoes).
- Incorporate animal sources such as liver (sparingly due to its high Vitamin A content), eggs, and fortified dairy products.
- Ensure adequate fat intake with meals to aid absorption of fat-soluble vitamins.
- Address Underlying Health Conditions: If you have a medical condition that affects nutrient absorption or metabolism (e.g., celiac disease, Crohn's, liver disease), work closely with your doctor to manage these conditions and monitor your nutritional status.
- Consult a Healthcare Professional Before Supplementing: Never self-diagnose or self-treat a Vitamin A deficiency or toxicity. If you suspect an issue or are considering supplementation, discuss it with your doctor or a registered dietitian. They can assess your individual needs, recommend appropriate testing, and guide you on safe and effective strategies.
Conclusion
Vitamin A is indisputably vital for health, playing a critical role in vision, immunity, and cellular function. Doctors order Vitamin A tests primarily when there is a clinical suspicion of deficiency or toxicity, or to monitor patients with chronic conditions that predispose them to altered Vitamin A status. Understanding the nuances of dietary sources, bioavailability, and the potential risks of inappropriate supplementation is paramount. Always rely on professional medical advice for diagnosis, treatment, and supplementation to ensure optimal health outcomes and prevent adverse effects.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin A levels?
The most common cause of abnormally low Vitamin A levels (deficiency) in developing countries is inadequate dietary intake. In developed countries, it is more frequently due to malabsorption syndromes (e.g., cystic fibrosis, celiac disease, Crohn's disease, chronic pancreatitis) or chronic liver disease, which impair the body's ability to absorb, store, or utilize Vitamin A. Abnormally high Vitamin A levels (toxicity or hypervitaminosis A) are almost exclusively caused by excessive intake of preformed Vitamin A supplements, rather than dietary sources alone.
How often should I get my Vitamin A tested?
For most healthy individuals without underlying medical conditions or symptoms of deficiency or toxicity, routine Vitamin A testing is not recommended. It is not a standard part of annual physical exams. Doctors typically order a Vitamin A test only when there's a strong clinical indication, such as unexplained symptoms suggestive of deficiency (like night blindness or recurrent infections), or toxicity (like severe headaches or skin changes), or as part of monitoring for specific chronic diseases (e.g., cystic fibrosis, post-bariatric surgery) that are known to affect Vitamin A status. The frequency of testing in these specific cases would be determined by the treating physician based on the patient's condition and response to treatment.
Can lifestyle changes improve my Vitamin A levels?
Yes, lifestyle changes, particularly dietary modifications, are highly effective in improving Vitamin A levels for individuals with dietary inadequacy.
- Dietary Diversity: Consuming a wide variety of foods rich in both preformed Vitamin A (e.g., liver, eggs, fortified dairy) and provitamin A carotenoids (e.g., carrots, sweet potatoes, spinach, kale) is the cornerstone of maintaining healthy levels.
- Fat Intake: Ensuring adequate dietary fat with meals is crucial for the absorption of fat-soluble Vitamin A. Including healthy fats like avocados, nuts, seeds, and olive oil can enhance absorption.
- Managing Underlying Conditions: For individuals with malabsorption issues or chronic diseases, adhering to medical treatment plans for those conditions is a critical "lifestyle change" that will indirectly improve Vitamin A absorption and utilization. This might include managing celiac disease with a gluten-free diet or treating pancreatic insufficiency.
- Limiting Alcohol Intake: Chronic alcohol abuse can impair liver function and nutrient absorption, so reducing or eliminating alcohol can support better Vitamin A status. These changes, when implemented consistently, can significantly contribute to maintaining or restoring optimal Vitamin A levels.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.