Low Hemoglobin (Anemia): Causes, Symptoms, and Treatments
Direct answer: Low hemoglobin, a condition known as anemia, means your blood has a reduced ability to carry oxygen. This often leads to symptoms like fatigue, weakness, and shortness of breath, and is typically caused by nutritional deficiencies, blood loss, or chronic diseases.
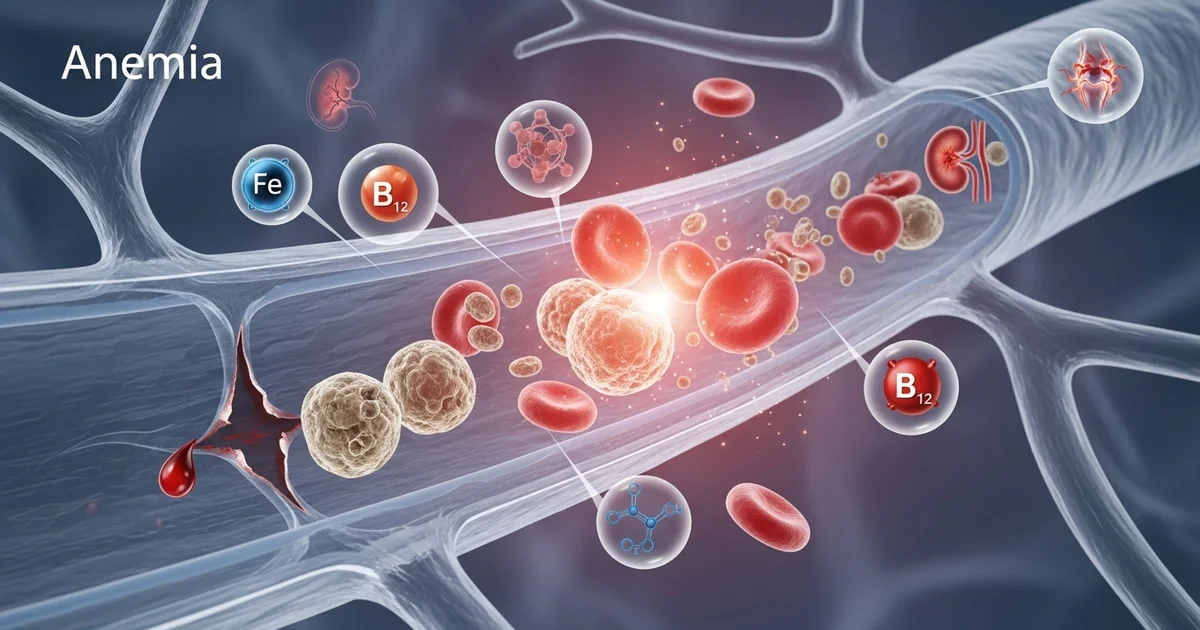
TL;DR Low hemoglobin, or anemia, occurs when your body lacks enough healthy red blood cells to transport oxygen effectively, leading to persistent fatigue and weakness. This common blood condition isn't a disease itself but a sign of an underlying issue. The most frequent causes are nutritional deficiencies, particularly a lack of iron, vitamin B12, or folate. Other major causes include chronic or acute blood loss (from heavy periods or internal bleeding), and various chronic diseases like kidney disease or inflammatory disorders that interfere with red blood cell production. Identifying the specific cause through blood tests is the first step toward effective treatment.
- Nutritional Deficiencies: The most common cause, especially iron deficiency. Lack of vitamin B12 and folate also leads to anemia.
- Blood Loss: Can be obvious (trauma, heavy periods) or hidden (slow gastrointestinal bleeding from ulcers or polyps).
- Chronic Diseases: Conditions like chronic kidney disease, rheumatoid arthritis, and cancer can disrupt red blood cell production.
- Bone Marrow Problems: Disorders like aplastic anemia or leukemia directly impair the body's ability to make blood cells.
- Hemolysis: This is the premature destruction of red blood cells, which can be caused by autoimmune conditions or genetic disorders.
- Genetic Conditions: Inherited disorders such as sickle cell anemia and thalassemia affect hemoglobin structure and function.
- Common Symptoms: Key signs include constant fatigue, pale skin, shortness of breath, dizziness, and cold hands or feet.
Want the full explanation? Keep reading ↓
Hemoglobin (Hb) is a critical protein found within red blood cells, playing an indispensable role in oxygen transport throughout the body. When hemoglobin levels fall below the normal range, a condition known as anemia ensues. Anemia is not a disease in itself but rather a sign of an underlying health issue, characterized by the body's reduced capacity to carry oxygen, leading to a myriad of symptoms ranging from mild fatigue to severe organ dysfunction. Understanding the causes and available treatments for low hemoglobin is crucial for effective management and improving quality of life.
What is Hemoglobin and Why is it Important?
Hemoglobin is a complex protein molecule rich in iron, primarily responsible for binding to oxygen in the lungs and delivering it to tissues and organs throughout the body. It also plays a role in transporting carbon dioxide back to the lungs to be exhaled. The characteristic red color of blood is due to hemoglobin. Without adequate hemoglobin, cells and tissues are deprived of the oxygen they need to function properly, impacting everything from energy levels to cognitive function. To delve deeper into its vital functions, you can explore our detailed article on [what is hemoglobin and its function in red blood cells].
Understanding Anemia
Anemia is clinically defined as a reduction in the total number of red blood cells or the amount of hemoglobin within them, leading to decreased oxygen-carrying capacity of the blood. It is one of the most common blood disorders globally, affecting millions of people across all age groups and demographics.
Symptoms of Low Hemoglobin (Anemia)
The symptoms of anemia can vary widely depending on the severity, the rate of onset, and the individual's overall health. Mild anemia may be asymptomatic, while severe cases can be debilitating. Common symptoms include:
- Fatigue and Weakness: The most prevalent symptom, resulting from insufficient oxygen reaching the muscles and tissues.
- Pale Skin, Gums, and Nail Beds: Reduced hemoglobin, which gives blood its red color, can make the skin appear paler.
- Shortness of Breath: Especially during exertion, as the body struggles to get enough oxygen.
- Dizziness or Lightheadedness: Due to reduced oxygen supply to the brain.
- Cold Hands and Feet: Poor circulation and oxygen delivery.
- Headaches: Often a result of decreased oxygen to the brain.
- Irregular Heartbeats (Palpitations): The heart works harder to compensate for the lack of oxygen.
- Brittle Nails: A sign of chronic iron deficiency anemia.
- Pica: Cravings for non-nutritive substances like ice, dirt, or clay, particularly common in iron deficiency.
- Restless Legs Syndrome: An uncomfortable sensation in the legs, often worse at night.
Normal Hemoglobin Levels
Hemoglobin levels are typically measured as part of a Complete Blood Count (CBC) test. Normal ranges can vary based on age, sex, and even geographic location, and slight variations exist between different laboratories. Generally, males have higher hemoglobin levels than females. It's important to consult with a healthcare professional to interpret your specific results within the context of your overall health. For a comprehensive overview of how these levels vary, refer to our article on [hemoglobin normal range by age and sex].
Here is a general guide to normal hemoglobin reference ranges:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 13.5-17.5 | g/dL | Varies slightly by lab |
| Adult Women | 12.0-15.5 | g/dL | Lower in premenopausal women due to menstruation |
| Pregnant Women | 11.0-14.0 | g/dL | Often lower due to hemodilution |
| Children (6-12 years) | 11.0-16.0 | g/dL | Age-dependent, generally increases with age |
| Infants (6 months-2 years) | 9.5-13.0 | g/dL | Varies significantly in infancy |
Note: These ranges are general guidelines. Your doctor will interpret your results based on your individual health profile and the specific reference ranges used by the laboratory.
Causes of Low Hemoglobin (Anemia)
Anemia can arise from three primary mechanisms: decreased red blood cell production, increased red blood cell destruction, or significant blood loss. Within these categories, numerous specific causes exist.
1. Nutritional Deficiencies
These are among the most common causes of anemia worldwide, particularly iron deficiency anemia.
- Iron Deficiency: Iron is a crucial component of hemoglobin synthesis. Without sufficient iron, the body cannot produce enough hemoglobin.
- Causes: Inadequate dietary intake (common in vegetarians/vegans if not carefully planned), chronic blood loss (menstruation, gastrointestinal bleeding), malabsorption (celiac disease, bariatric surgery), increased demand (pregnancy, rapid growth in children).
- Vitamin B12 Deficiency (Megaloblastic Anemia): Vitamin B12 is essential for DNA synthesis in red blood cell production.
- Causes: Pernicious anemia (autoimmune condition preventing B12 absorption), strict vegan diet, malabsorption disorders (Crohn's disease, gastric surgery), certain medications (e.g., metformin, proton pump inhibitors).
- Folate (Folic Acid) Deficiency (Megaloblastic Anemia): Similar to B12, folate is vital for DNA synthesis and red blood cell maturation.
- Causes: Inadequate dietary intake (found in leafy greens, fruits), malabsorption, increased demand (pregnancy), chronic alcohol abuse, certain medications (e.g., methotrexate).
2. Blood Loss
Significant blood loss, whether acute or chronic, can rapidly deplete the body's iron stores and lead to anemia.
- Acute Blood Loss:
- Trauma or Surgery: Major injuries or surgical procedures can result in substantial blood loss.
- Gastrointestinal Bleeding: Ulcers, hemorrhoids, diverticulosis, inflammatory bowel disease, or certain cancers can cause acute or chronic bleeding, often unnoticed.
- Chronic Blood Loss:
- Heavy Menstrual Periods (Menorrhagia): A very common cause of iron deficiency anemia in premenopausal women.
- Gastrointestinal Bleeding: Slow, persistent bleeding from conditions like polyps, gastritis, or colon cancer can lead to gradual iron depletion.
- Frequent Blood Donations: While generally safe, very frequent donations can contribute to iron deficiency over time.
3. Chronic Diseases
Several chronic medical conditions can interfere with red blood cell production or survival.
- Anemia of Chronic Disease (ACD) / Anemia of Inflammation: Often seen in individuals with chronic infections (e.g., HIV/AIDS), inflammatory diseases (e.g., rheumatoid arthritis, lupus), or cancer. The inflammation interferes with iron utilization and red blood cell production.
- Chronic Kidney Disease: Damaged kidneys may not produce enough erythropoietin, a hormone vital for stimulating red blood cell production in the bone marrow.
- Cancer: Cancers can cause anemia through various mechanisms:
- Direct invasion of bone marrow.
- Chronic blood loss (e.g., colorectal cancer).
- Inflammation and cytokine production.
- Side effects of chemotherapy or radiation.
- Liver Disease: The liver produces factors necessary for red blood cell production and metabolism. Chronic liver disease can lead to anemia.
4. Bone Marrow Disorders
The bone marrow is the factory for all blood cells. Problems here directly impact hemoglobin levels.
- Aplastic Anemia: A rare but severe condition where the bone marrow stops producing enough new blood cells, including red blood cells.
- Myelodysplastic Syndromes (MDS): A group of disorders where the bone marrow produces abnormal or immature blood cells that don't mature properly.
- Leukemia and Lymphoma: Cancers of the blood and bone marrow can crowd out normal blood-forming cells.
- Myelofibrosis: A rare bone marrow cancer where scar tissue replaces normal bone marrow, impairing blood cell production.
5. Hemolytic Anemias
These occur when red blood cells are destroyed faster than the bone marrow can produce them.
- Autoimmune Hemolytic Anemia: The immune system mistakenly attacks and destroys red blood cells.
- Drug-Induced Hemolytic Anemia: Certain medications can trigger red blood cell destruction.
- Mechanical Hemolysis: Artificial heart valves or other medical devices can cause physical damage to red blood cells.
- Infections: Some infections, like malaria, can directly destroy red blood cells.
6. Genetic Conditions
Inherited disorders can affect the structure or production of hemoglobin.
- Thalassemia: A group of inherited blood disorders characterized by abnormal hemoglobin production, leading to reduced hemoglobin and red blood cell count.
- Sickle Cell Anemia: An inherited disorder where red blood cells become crescent-shaped, rigid, and prone to breaking down prematurely, leading to chronic anemia and pain crises.
- G6PD Deficiency: A genetic condition that makes red blood cells vulnerable to oxidative stress, leading to hemolysis when exposed to certain foods, drugs, or infections.
7. Other Causes
- Pregnancy: The increased blood volume during pregnancy dilutes red blood cells, often leading to physiological anemia. Iron and folate requirements also significantly increase.
- Alcohol Abuse: Chronic alcohol consumption can interfere with nutrient absorption (especially folate and B12), suppress bone marrow activity, and cause gastrointestinal bleeding.
- Lead Poisoning: Lead can interfere with heme synthesis, leading to anemia.
Diagnosing Low Hemoglobin
Diagnosis typically begins with a Complete Blood Count (CBC), which measures hemoglobin, hematocrit (the percentage of red blood cells in the blood), red blood cell count, and other parameters. If low hemoglobin is detected, further tests are usually ordered to determine the underlying cause:
- Iron Studies: Ferritin (iron stores), serum iron, total iron-binding capacity (TIBC), transferrin saturation.
- Vitamin B12 and Folate Levels.
- Kidney and Liver Function Tests.
- Thyroid Function Tests.
- Stool Guaiac Test: To check for occult blood in stool (indicating GI bleeding).
- Endoscopy or Colonoscopy: If GI bleeding is suspected.
- Bone Marrow Biopsy: In cases of suspected bone marrow disorders.
- Genetic Testing: For inherited anemias like thalassemia or sickle cell disease.
Treatments for Low Hemoglobin
Treatment for low hemoglobin is highly dependent on the underlying cause. Addressing the root issue is paramount for successful management.
1. Nutritional Supplementation
- Iron Supplements: For iron deficiency anemia, oral iron supplements (ferrous sulfate, ferrous gluconate) are the first-line treatment. In severe cases, or if oral supplements are not tolerated or absorbed, intravenous (IV) iron infusions may be necessary. It's crucial to take iron as directed, often with vitamin C to enhance absorption, and to be aware of potential side effects like constipation or stomach upset.
- Vitamin B12 Injections or Oral Supplements: For B12 deficiency, particularly in pernicious anemia or malabsorption, B12 injections are typically administered initially, followed by regular maintenance doses. High-dose oral supplements may be effective for some causes.
- Folic Acid Supplements: For folate deficiency, oral folic acid supplements are usually very effective.
2. Addressing Blood Loss
- Identifying and Stopping Bleeding: This is critical. Treatment may involve medications for ulcers, surgical intervention for severe bleeding, or management of heavy menstrual bleeding (e.g., hormonal therapy, endometrial ablation).
- Management of Chronic Conditions: Controlling underlying conditions like inflammatory bowel disease can reduce associated blood loss.
3. Treating Underlying Chronic Diseases
- Erythropoietin-Stimulating Agents (ESAs): For anemia of chronic kidney disease or certain cancers, synthetic erythropoietin can stimulate the bone marrow to produce more red blood cells.
- Management of Inflammatory Conditions: Treating the underlying inflammation in conditions like rheumatoid arthritis can improve anemia of chronic disease.
- Cancer Treatment: Successful treatment of cancer can often resolve associated anemia.
4. Blood Transfusions
- Red Blood Cell Transfusions: In severe cases of anemia, especially when symptoms are debilitating or there's acute blood loss, blood transfusions may be necessary to rapidly increase hemoglobin levels and improve oxygen-carrying capacity. This is a temporary measure and doesn't address the underlying cause.
5. Medications and Procedures for Specific Anemias
- Immunosuppressants: For autoimmune hemolytic anemia, medications that suppress the immune system may be used.
- Splenectomy: In some types of hemolytic anemia where the spleen is overactive in destroying red blood cells, surgical removal of the spleen may be considered.
- Bone Marrow Transplant: For severe aplastic anemia, myelodysplastic syndromes, or certain leukemias.
- Chelation Therapy: For thalassemia major, to remove excess iron that accumulates from frequent blood transfusions.
Living with Low Hemoglobin: Actionable Advice
While medical treatment is essential, certain lifestyle adjustments can support recovery and help manage symptoms.
- Dietary Choices:
- Iron-Rich Foods: Incorporate lean red meat, poultry, fish, beans, lentils, spinach, fortified cereals, and dried fruits.
- Vitamin C: Consume foods high in vitamin C (citrus fruits, bell peppers, broccoli) with iron-rich meals to enhance iron absorption.
- Folate-Rich Foods: Leafy green vegetables, fortified grains, beans, and oranges.
- Vitamin B12-Rich Foods: Meat, fish, poultry, eggs, dairy products, and fortified foods (for vegans).
- Avoid Iron Absorption Inhibitors: Limit consumption of coffee, tea, and calcium-rich foods or supplements around the time you take iron supplements, as they can hinder absorption.
- Regular Exercise: Gentle, consistent exercise can improve circulation and energy levels, but avoid overexertion, especially if anemic symptoms are severe.
- Adequate Rest: Prioritize sleep and allow for rest periods throughout the day to combat fatigue.
- Stay Hydrated: While dehydration can lead to artificially high hemoglobin readings, maintaining good hydration is important for overall health. Interestingly, high hemoglobin levels can sometimes be a sign of dehydration, as discussed in our article on [high hemoglobin levels, dehydration, smoking, and polycythemia].
- Follow Medical Advice: Adhere strictly to your doctor's treatment plan, including medication dosages and follow-up appointments.
When to See a Doctor
If you experience persistent symptoms of fatigue, weakness, paleness, shortness of breath, or dizziness, it is crucial to consult a healthcare professional. Early diagnosis and treatment of low hemoglobin can prevent complications and improve your overall health and well-being. Do not self-diagnose or self-treat, as the underlying cause needs to be accurately identified.
Frequently Asked Questions
What is the most common cause of abnormal Hemoglobin (Hb) levels?
The most common cause of abnormally low hemoglobin levels (anemia) worldwide is iron deficiency. This is often due to inadequate dietary iron intake, chronic blood loss (such as heavy menstrual periods or gastrointestinal bleeding), or impaired iron absorption. For abnormally high hemoglobin levels, dehydration is a common temporary cause, while conditions like polycythemia vera can cause persistently elevated levels.
How often should I get my Hemoglobin (Hb) tested?
The frequency of hemoglobin testing depends on individual health status, risk factors, and existing medical conditions. For healthy adults without known risk factors for anemia, routine physical exams that include a Complete Blood Count (CBC) typically occur every 1-3 years. However, if you have symptoms of anemia, a chronic disease (like kidney disease or inflammatory conditions), are pregnant, or have a history of anemia, your doctor may recommend more frequent testing, ranging from every few months to annually, to monitor your levels and the effectiveness of treatment.
Can lifestyle changes improve my Hemoglobin (Hb) levels?
Yes, lifestyle changes can significantly improve hemoglobin levels, especially when the underlying cause is nutritional deficiency. Consuming a diet rich in iron (red meat, beans, spinach), vitamin B12 (meat, dairy, fortified foods), and folate (leafy greens, fortified grains) is crucial. Pairing iron-rich foods with vitamin C can enhance iron absorption. Additionally, avoiding substances that inhibit iron absorption (like coffee and tea with meals) and managing chronic conditions that contribute to anemia are important. While lifestyle changes are powerful, they should always complement, not replace, medical treatment and advice from your healthcare provider.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.