Understanding Your Blood Test: A Clear Guide to RBC Indices
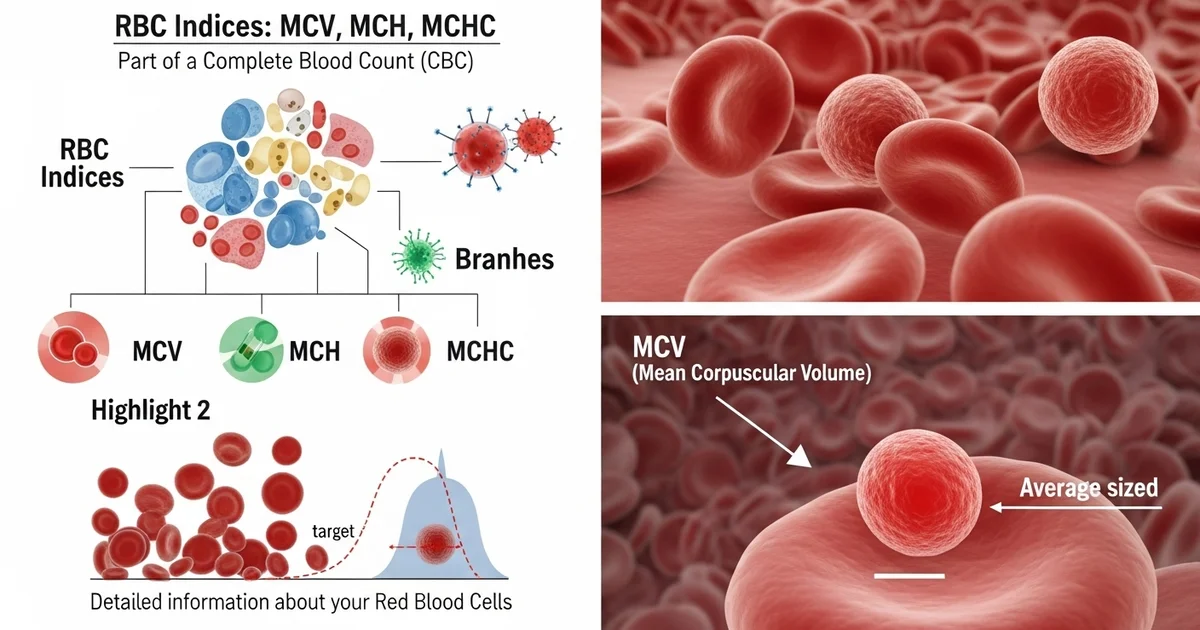
Direct answer: RBC indices—MCV, MCH, and MCHC—are part of a complete blood count (CBC) that provide detailed information about your red blood cells. MCV (Mean Corpuscular Volume) measures the average size of your red blood cells. MCH (Mean Corpuscular Hemoglobin) measures the average amount of hemoglobin per red blood cell. MCHC (Mean Corpuscular Hemoglobin Concentration) measures the concentration of hemoglobin in a given volume of red blood cells. These values help diagnose different types of anemia and other conditions.
TL;DR RBC indices are specific measurements that tell a story about the health, size, and hemoglobin content of your red blood cells. Included in a standard complete blood count (CBC), these values—MCV, MCH, and MCHC—help your doctor look beyond a simple red blood cell count to diagnose conditions like anemia, thalassemia, and other disorders. Understanding what they measure is the first step to making sense of your lab report and having more informed conversations with your healthcare provider.
MCV (Mean Corpuscular Volume): This measures the average size of your red blood cells. High MCV can indicate a vitamin B12 or folate deficiency, while low MCV may suggest iron deficiency anemia or thalassemia.
MCH (Mean Corpuscular Hemoglobin): This measures the average amount of hemoglobin—the protein that carries oxygen—inside a single red blood cell. Its value often mirrors the MCV result, as larger cells typically hold more hemoglobin.
MCHC (Mean Corpuscular Hemoglobin Concentration): This measures the concentration of hemoglobin within a red blood cell. Low MCHC means the cells are pale (hypochromic), often seen in iron deficiency. High MCHC is less common but can point to certain hereditary conditions.
Why They Matter: Abnormalities in these indices are crucial clues for doctors. For example, low values across MCV, MCH, and MCHC often point towards iron deficiency anemia, the most common type.
The Big Picture: These indices are never interpreted in isolation. Your doctor will analyze them alongside your total RBC count, hemoglobin, hematocrit, and other CBC results to get a complete picture of your blood health.
Next Steps: If your results are outside the normal range, your doctor will explain what they mean for you and may order follow-up tests to confirm a diagnosis and create a treatment plan.
Want the full explanation? Keep reading ↓
Got Your Blood Test Results? Understanding What RBC Indices Mean for Your Health
Your Complete Blood Count (CBC) report is packed with valuable information, but the acronyms can be confusing. Beyond the basic red blood cell count, your report includes a critical set of measurements called Red Blood Cell (RBC) indices: MCV, MCH, and MCHC. These indices provide a detailed look at the size, weight, and hemoglobin concentration of your individual red blood cells.
Think of it this way: while the [RBC count tells you how many red blood cells you have], the indices tell you about the quality and characteristics of those cells. This information is crucial for diagnosing and classifying different types of anemia and other blood disorders, often before more obvious symptoms appear. Understanding these values is the key to unlocking a deeper understanding of your health.
This article will break down each RBC index, explaining what it measures, what high or low values could mean, and how they work together to paint a complete picture of your red blood cell health.
Feeling Fatigued? Your MCV Might Hold the Answer
Mean Corpuscular Volume (MCV) is arguably the most important of the RBC indices. It measures the average size or volume of your red blood cells. It's the first clue a healthcare provider uses to classify anemia.
The MCV value helps categorize red blood cells into one of three types:
- Normocytic: Normal size
- Microcytic: Smaller than normal
- Macrocytic: Larger than normal
This classification is the first step in narrowing down the potential causes of anemia or other blood conditions.
What Does a Low MCV (Microcytosis) Mean?
If your red blood cells are smaller than average (microcytic), it means they are not being produced correctly. The most common reason for this is a problem with hemoglobin production, the protein that carries oxygen.
Common causes of a low MCV include:
- Iron Deficiency Anemia: This is the most common cause of microcytic anemia worldwide. Without enough iron, your body cannot produce enough hemoglobin, leading to smaller, paler red blood cells.
- Thalassemia: A group of genetic disorders that affect hemoglobin production. The severity can range from mild (alpha or beta thalassemia minor) to severe.
- Anemia of Chronic Disease/Inflammation: Long-term illnesses (like rheumatoid arthritis, Crohn's disease, or chronic kidney disease) can interfere with the body's ability to use iron, leading to microcytic anemia over time.
- Sideroblastic Anemia: A rare disorder where the body has iron but cannot incorporate it into hemoglobin properly, leading to iron accumulation in the mitochondria of red blood cell precursors.
- Lead Poisoning: Lead can disrupt multiple steps in hemoglobin synthesis, causing microcytic anemia.
Why Is Your MCV High? Understanding Macrocytosis
When red blood cells are larger than average (macrocytic), it usually points to a problem with the cell division and maturation process in the bone marrow.
Common causes of a high MCV include:
- Vitamin B12 Deficiency: Vitamin B12 is essential for DNA synthesis. Without it, cell division is impaired, and red blood cells are released from the bone marrow while they are still large and immature. This is often seen in pernicious anemia or in individuals with vegan diets who do not supplement.
- Folate (Vitamin B9) Deficiency: Similar to B12, folate is crucial for DNA synthesis. A deficiency has the same effect, leading to macrocytic anemia.
- Liver Disease: Chronic liver disease can affect the lipid composition of red blood cell membranes, causing them to appear larger.
- Alcoholism: Excessive alcohol consumption is directly toxic to bone marrow and can also interfere with the absorption and metabolism of folate, leading to a high MCV.
- Hypothyroidism: An underactive thyroid can cause a range of changes in the CBC, including, in some cases, a high MCV.
- Certain Medications: Some drugs, including chemotherapy agents (like methotrexate) and certain antivirals, can interfere with DNA synthesis and cause a high MCV.
Is Your MCH a Helpful Clue? What This Index Reveals
Mean Corpuscular Hemoglobin (MCH) measures the average amount, or weight, of hemoglobin in each red blood cell. It essentially tells you how "heavy" the average red blood cell is with hemoglobin.
The MCH value is calculated from the hemoglobin and red blood cell count. Because it is highly dependent on the average cell size (MCV), it often rises or falls in tandem with the MCV. For this reason, many clinicians find it less useful than the MCV and MCHC for differential diagnosis.
- Low MCH: Often seen in microcytic anemias like iron deficiency, where cells are both small and contain less hemoglobin.
- High MCH: Typically seen in macrocytic anemias, where the larger cells can physically hold more hemoglobin, even if the concentration is normal.
While it provides some information, it's rare for a diagnosis to be based on an MCH value that is inconsistent with the MCV. The MCHC is often considered a more reliable measure of hemoglobin content.
Pale or Packed? What MCHC Reveals About Hemoglobin Concentration
Mean Corpustular Hemoglobin Concentration (MCHC) measures the average concentration of hemoglobin within a given volume of packed red blood cells. Instead of the weight of hemoglobin per cell (MCH), it tells you how concentrated the hemoglobin is.
Think of MCH as the total sugar in a cookie, while MCHC is how sweet the cookie tastes. A very large cookie (high MCV) might have more sugar overall (high MCH) but taste bland if the sugar isn't concentrated (normal MCHC).
The MCHC helps classify red blood cells as:
- Normochromic: Normal hemoglobin concentration (cells have a normal reddish color).
- Hypochromic: Low hemoglobin concentration (cells appear paler).
- Hyperchromic: High hemoglobin concentration (cells appear darker and more saturated).
What Does a Low MCHC (Hypochromia) Suggest?
A low MCHC indicates that your red blood cells have a lower concentration of hemoglobin than normal, making them appear "hypochromic" or pale. This finding is a classic hallmark of certain conditions.
Primary causes of a low MCHC include:
- Iron Deficiency Anemia: As iron stores are depleted, the bone marrow produces cells that are not only smaller (low MCV) but also have a lower concentration of hemoglobin (low MCHC).
- Thalassemia: Similar to iron deficiency, the impaired hemoglobin production in thalassemia leads to cells with a lower hemoglobin concentration.
A low MCHC combined with a low MCV is a very strong indicator of either iron deficiency or thalassemia.
Can Your MCHC Be Too High? Understanding Hyperchromia
A truly high MCHC is rare. The red blood cell has a physiological limit to how much hemoglobin it can hold before the cell becomes unstable. Therefore, a high MCHC value should always be interpreted with caution, as it can be a true pathological finding or an artifact.
Potential causes of a high MCHC include:
- Hereditary Spherocytosis: A genetic condition where a defect in the red blood cell membrane causes the cell to become spherical rather than the usual biconcave disc. These smaller, denser cells have a genuinely high hemoglobin concentration.
- Autoimmune Hemolytic Anemia: Certain types of this condition can lead to the formation of spherocytes, also increasing the MCHC.
- Severe Burns: Can sometimes lead to cellular dehydration and an artificially high MCHC.
- Sample Artifact (Most Common): A high MCHC is often not a true result. It can be caused by factors like cold agglutinins (antibodies that cause RBCs to clump at cold temperatures), lipemia (high levels of fat in the blood), or hemolysis (rupturing of red blood cells in the sample). Automated analyzers may misread these clumped or altered samples, generating a falsely elevated MCHC.
Connecting the Dots: How RBC Indices Work Together to Diagnose Anemia
The real diagnostic power of RBC indices comes from looking at them together. By combining the MCV, MCH, and MCHC, a clinician can quickly narrow down the list of possible causes for a patient's anemia.
This table shows how different patterns of RBC indices point toward specific diagnoses:
| Condition / Anemia Type | MCV (Size) | MCHC (Concentration) | Common Causes & Notes |
|---|---|---|---|
| Iron Deficiency Anemia | Low | Low | The most common pattern. Cells are small (microcytic) and pale (hypochromic). |
| Thalassemia | Very Low | Low or Normal | MCV is often disproportionately low compared to the degree of anemia. |
| Anemia of Chronic Disease | Normal or Low | Normal | Starts as normocytic/normochromic and can become microcytic over time. |
| Acute Blood Loss | Normal | Normal | The body loses whole blood, so the remaining cells are normal in size and color. Indices only change if deficiency develops over time. |
| B12/Folate Deficiency | High | Normal | The classic "macrocytic anemia." Cells are large, but hemoglobin concentration is usually normal. |
| Hereditary Spherocytosis | Normal or Low | High | This is the hallmark finding for this condition. The high MCHC is a key diagnostic clue. |
Understanding these patterns is essential. For example, if a patient has anemia with a low MCV and low MCHC, the first step is to investigate for iron deficiency. If the anemia features a high MCV and normal MCHC, the focus shifts to B12 and folate levels. Sometimes an unusually high number of red blood cells can also point to specific conditions, and it is important to understand the risks associated with a [high RBC count, or erythrocytosis].
RBC Indices: Reference Ranges
Reference ranges for RBC indices can vary slightly between laboratories, but the following table provides typical values for adults. It's important to compare your results to the specific range provided on your lab report. For a more detailed breakdown, you can explore the [normal RBC count ranges for adults and kids] to see how these values change with age.
| Index | Normal Range | Units | Notes |
|---|---|---|---|
| MCV | 80 - 100 | fL | Femtoliters; measures average red blood cell size. |
| MCH | 27 - 34 | pg | Picograms; measures average hemoglobin weight per red blood cell. |
| MCHC | 32 - 36 | g/dL | Grams per deciliter; measures hemoglobin concentration within red blood cells. |
| RDW | 11.5 - 14.5 | % | Red Cell Distribution Width; measures the variation in RBC size (not an index, but related). |
Note: The RDW (Red Cell Distribution Width) is another important parameter often reported with RBC indices. It measures the variation in the size of your red blood cells. A high RDW means there is a large variation in cell size (anisocytosis) and is an early indicator of conditions like iron deficiency.
What Should You Do If Your RBC Indices Are Abnormal?
If one or more of your RBC indices are outside the normal range, it's important not to panic. An abnormal result is a starting point for a conversation with your healthcare provider, not a final diagnosis.
Actionable steps to take:
- Consult Your Doctor: Schedule an appointment to discuss your results. Your doctor will interpret them in the context of your overall health, symptoms, and other lab work.
- Prepare for Follow-Up Tests: Your doctor may order additional tests to confirm a diagnosis. These could include:
- Iron Panel: Ferritin, serum iron, TIBC
- Vitamin Levels: Vitamin B12 and Folate
- Hemoglobin Electrophoresis: To test for thalassemia or sickle cell disease
- Reticulocyte Count: To check if your bone marrow is producing new red blood cells effectively
- Discuss Your Diet and Lifestyle: Be prepared to talk about your diet, alcohol consumption, medications, and any chronic health conditions. These factors are critical for an accurate diagnosis.
- Follow Your Treatment Plan: If a diagnosis is made, your treatment will depend on the underlying cause. It may be as simple as taking iron or vitamin supplements, or it may involve managing a chronic condition more effectively.
Your RBC indices are powerful tools in preventive and diagnostic medicine. By understanding what they measure, you can become a more informed and proactive partner in your own healthcare journey.
Frequently Asked Questions
What is the most common cause of abnormal Red Blood Cell Count (RBC) levels?
The most common cause of abnormal RBC indices, specifically a low MCV and low MCHC, is iron deficiency anemia. This condition is widespread globally and affects individuals of all ages, particularly premenopausal women, pregnant women, young children, and individuals with dietary restrictions or malabsorption issues like celiac disease. The body requires iron to produce hemoglobin, and without enough of it, the bone marrow produces red blood cells that are small (microcytic) and pale (hypochromic), leading to these characteristic index abnormalities.
How often should I get my Red Blood Cell Count (RBC) tested?
The frequency of testing depends entirely on your individual health situation. For healthy adults with no symptoms or chronic diseases, an RBC count and indices are typically checked as part of a routine physical exam every 1 to 3 years. However, if you have a known blood disorder (like anemia), are undergoing treatment that can affect blood cells (like chemotherapy), are pregnant, or have a chronic condition (like kidney disease or an inflammatory disorder), your doctor may recommend testing much more frequently—from every few weeks to every few months—to monitor your condition and the effectiveness of treatment.
Can lifestyle changes improve my Red Blood Cell Count (RBC) levels?
Yes, in many cases, lifestyle changes can significantly improve RBC indices, especially when the abnormality is caused by a nutritional deficiency. Key changes include:
- Dietary Adjustments: Consuming a diet rich in iron (red meat, poultry, beans, lentils, spinach), vitamin B12 (animal products, fortified cereals), and folate (leafy greens, citrus fruits, beans) can prevent and treat the most common forms of anemia.
- Limiting Alcohol: Reducing excessive alcohol intake can improve high MCV, as alcohol is toxic to the bone marrow and interferes with folate absorption.
- Managing Chronic Conditions: Effectively managing chronic diseases like diabetes, autoimmune disorders, or kidney disease can help resolve "anemia of chronic disease" and normalize RBC indices.
- Proper Supplementation: If you follow a diet that excludes certain food groups (e.g., veganism and B12), taking appropriate supplements as advised by a healthcare provider is crucial.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.