Low Hematocrit: Causes, Symptoms, and Connection to Anemia
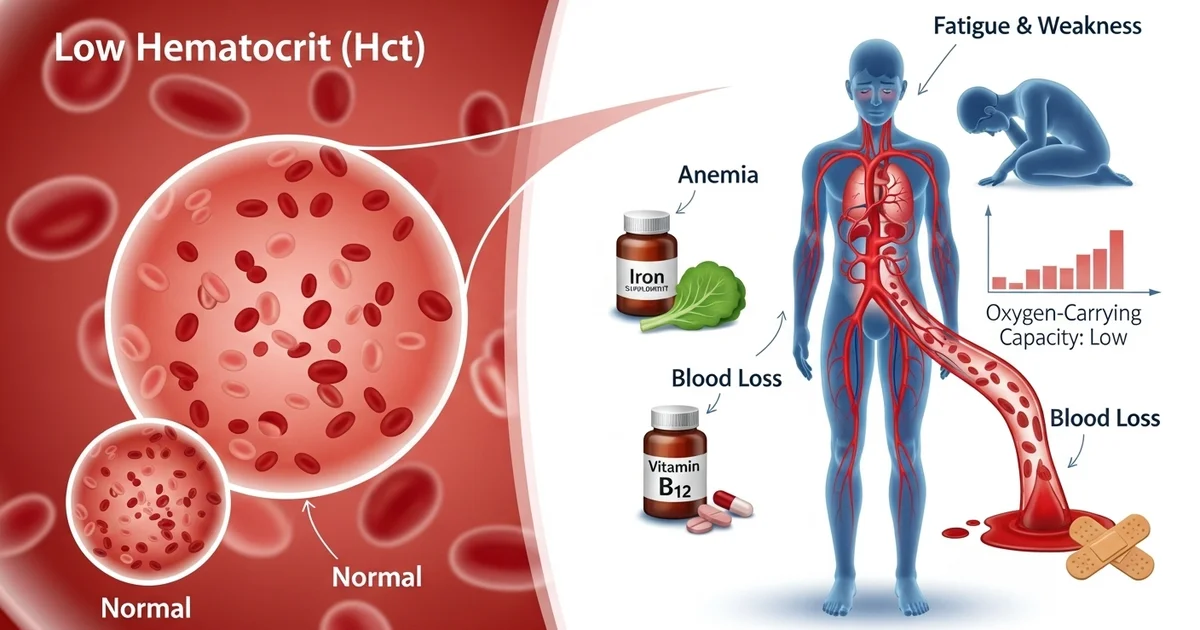
Direct answer: A low hematocrit (Hct) level means the percentage of red blood cells in your blood is below normal, reducing its oxygen-carrying capacity. This is most commonly caused by anemia (often from iron or vitamin deficiency) or significant blood loss, leading to symptoms like fatigue and weakness.
TL;DR A low hematocrit (Hct) indicates that you have a lower-than-normal volume of red blood cells, which are essential for carrying oxygen throughout your body. This condition is a primary indicator of anemia or significant blood loss. When your hematocrit is low, your body's tissues may not get enough oxygen, leading to common symptoms like persistent fatigue, weakness, shortness of breath, and pale skin. The causes are diverse, ranging from nutritional deficiencies to more serious underlying health issues.
- It's a key sign of anemia: Most often, low hematocrit points to anemia. This can be due to a lack of iron, vitamin B12, or folate, which are all necessary for producing healthy red blood cells.
- Blood loss is a direct cause: Both sudden (acute) blood loss from injury or surgery and slow (chronic) blood loss from conditions like heavy periods or gastrointestinal bleeding will lower your hematocrit.
- Chronic diseases can be the culprit: Conditions like chronic kidney disease, inflammatory disorders, and certain cancers can interfere with your body's ability to produce red blood cells, leading to low Hct.
- Bone marrow problems are a possibility: Disorders that affect the bone marrow, such as aplastic anemia or leukemia, can impair the production of all blood cells, including red blood cells.
- Symptoms are tied to low oxygen: The most common symptoms—fatigue, weakness, dizziness, pale skin, and shortness of breath—all result from your body's tissues being deprived of adequate oxygen.
- Diagnosis requires further testing: A low hematocrit result is a starting point. Your doctor will use this finding to order further tests to identify the specific underlying cause and determine the right treatment plan.
Want the full explanation? Keep reading ↓
Hematocrit (Hct) is a crucial component of a complete blood count (CBC), providing a snapshot of your red blood cell volume. It represents the percentage of your total blood volume that is made up of red blood cells. When your hematocrit levels drop below the normal range, it’s medically referred to as low hematocrit, a condition that often signals underlying health issues, most notably anemia or significant blood loss. Understanding the implications of a low hematocrit is vital for accurate diagnosis and effective treatment.
This article delves into the intricacies of low hematocrit, exploring its profound connections to anemia and various forms of blood loss, while also touching upon other potential causes and the diagnostic steps involved.
What is Hematocrit?
Hematocrit is a direct measure of the proportion of red blood cells in your blood. These vital cells, also known as erythrocytes, are responsible for transporting oxygen from your lungs to tissues and organs throughout your body and carrying carbon dioxide back to the lungs to be exhaled. A balanced hematocrit level ensures efficient oxygen delivery, which is fundamental for energy production and overall bodily function.
The hematocrit test is typically performed as part of a routine [complete blood count (CBC)]. During this test, a blood sample is taken, and the red blood cells are separated from the plasma and other blood components. The volume occupied by the red blood cells is then measured and expressed as a percentage of the total blood volume. This percentage provides an indirect but reliable indicator of the number of red blood cells and their oxygen-carrying capacity.
Understanding Low Hematocrit
A low hematocrit indicates that the percentage of red blood cells in your blood is lower than what is considered healthy for your age, sex, and other physiological factors. This reduction means your blood has a diminished capacity to carry oxygen, leading to a host of symptoms and potentially serious health complications if left unaddressed.
When Hct levels are low, it often points directly to anemia, a condition characterized by a reduced number of healthy red blood cells or a decrease in the amount of hemoglobin (the iron-rich protein that carries oxygen) within them. It can also be a critical indicator of recent or ongoing blood loss, where the body is losing red blood cells faster than it can produce them.
Normal Hematocrit Levels
Normal hematocrit levels vary significantly depending on several factors, including age, sex, and even altitude. Generally, men tend to have higher hematocrit levels than women, and newborns have particularly high levels that decrease during early infancy. Pregnancy can also influence hematocrit due to increased blood volume, which can dilute the red blood cell concentration.
It's important to note that these ranges are general guidelines, and individual laboratory values may differ slightly. Your healthcare provider will interpret your results in the context of your overall health, symptoms, and medical history. You can find more detailed information on specific ranges and their interpretation in our article on [normal hematocrit levels].
Here is a general reference range table for hematocrit:
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 40-54 | % | Varies slightly by lab and altitude |
| Adult Women | 36-48 | % | May be lower in pregnancy or menstruating |
| Children (Age 6-12) | 35-45 | % | Highly age-dependent; consult pediatrician for specifics |
| Newborns | 45-65 | % | Significantly higher at birth, then decreases |
A hematocrit value below the lower limit of the normal range is considered low and warrants further investigation.
The Connection to Anemia
Anemia is a condition in which your blood lacks healthy red blood cells, leading to reduced oxygen delivery to your body's tissues. A low hematocrit is often the primary laboratory finding that signals the presence of anemia. When your Hct is low, it directly reflects a deficiency in the oxygen-carrying capacity of your blood.
Anemia is not a single disease but rather a symptom of an underlying problem. Various types of anemia can lead to a low hematocrit:
- Iron-Deficiency Anemia: This is the most common type of anemia worldwide. It occurs when your body doesn't have enough iron to produce hemoglobin, which is essential for red blood cell function. Causes include inadequate dietary iron intake, chronic blood loss (e.g., heavy menstrual periods, gastrointestinal bleeding), malabsorption of iron, or increased iron requirements (e.g., pregnancy).
- Vitamin Deficiency Anemias:
- Vitamin B12 Deficiency Anemia (Pernicious Anemia): Caused by a lack of vitamin B12, often due to insufficient dietary intake (common in vegans) or the body's inability to absorb B12 (e.g., due to autoimmune conditions affecting the stomach lining, called pernicious anemia). B12 is crucial for red blood cell maturation.
- Folate Deficiency Anemia: Similar to B12 deficiency, a lack of folate (vitamin B9) can impair red blood cell production. It can result from poor diet, malabsorption, or increased demand (e.g., pregnancy).
- Anemia of Chronic Disease: Certain chronic inflammatory conditions, infections, cancers, and autoimmune diseases can interfere with red blood cell production, leading to a mild to moderate anemia. The body may have sufficient iron stores, but it cannot effectively utilize them.
- Aplastic Anemia: A rare but serious condition where the bone marrow fails to produce enough new blood cells, including red blood cells, white blood cells, and platelets. It can be caused by autoimmune disorders, exposure to toxins, certain medications, or viral infections.
- Hemolytic Anemia: This type occurs when red blood cells are destroyed faster than the bone marrow can produce them. Causes include autoimmune conditions, genetic disorders, infections, or reactions to certain medications or toxins.
- Genetic Anemias: Conditions like Sickle Cell Anemia and Thalassemia are inherited disorders that affect the structure or production of hemoglobin, leading to fragile or improperly formed red blood cells that are prematurely destroyed.
The symptoms of anemia, directly related to the reduced oxygen supply, include fatigue, weakness, pallor (pale skin), shortness of breath, dizziness, cold hands and feet, headaches, and irregular heartbeats (tachycardia).
The Connection to Blood Loss
Blood loss, whether acute and sudden or chronic and insidious, is a significant and often direct cause of low hematocrit.
Acute Blood Loss
Acute blood loss refers to a rapid and substantial loss of blood over a short period. This can lead to an immediate drop in the total volume of blood in the body, and consequently, a reduction in hematocrit. However, it's important to note that immediately after acute blood loss, the hematocrit might not drop significantly if the body hasn't yet had time to replace the lost plasma volume. The drop becomes more apparent as fluids shift from the tissues into the bloodstream to restore blood volume, thereby diluting the remaining red blood cells.
Common causes of acute blood loss include:
- Trauma: Severe injuries from accidents, falls, or violence can cause significant internal or external bleeding.
- Surgery: Blood loss during surgical procedures is expected, and excessive loss can lead to low Hct.
- Gastrointestinal (GI) Bleeding: Conditions like bleeding ulcers, esophageal varices, diverticulitis, or inflammatory bowel disease can result in sudden and heavy GI bleeding.
- Severe Epistaxis (Nosebleeds): While often minor, severe and prolonged nosebleeds can occasionally lead to significant blood loss.
- Childbirth Complications: Postpartum hemorrhage can cause a rapid drop in hematocrit.
Symptoms of acute blood loss are often dramatic and include rapid heart rate, low blood pressure, dizziness, fainting, shortness of breath, and pale, clammy skin.
Chronic Blood Loss
Chronic blood loss involves a slow, persistent loss of small amounts of blood over an extended period. Because the loss is gradual, the body may initially try to compensate by increasing red blood cell production. However, if the blood loss continues, the body's iron stores become depleted, eventually leading to iron-deficiency anemia and a sustained low hematocrit.
Sources of chronic blood loss are often subtle and may go unnoticed for a long time:
- Menorrhagia (Heavy Menstrual Bleeding): Women with excessively heavy or prolonged menstrual periods can lose significant amounts of blood each month, leading to chronic iron deficiency and low hematocrit.
- Gastrointestinal Bleeding: This is a very common cause of chronic blood loss. Conditions such as:
- Peptic ulcers
- Hiatal hernias
- Colon polyps
- Diverticulosis
- Inflammatory bowel disease (Crohn's disease, ulcerative colitis)
- Cancers of the GI tract
- Regular use of non-steroidal anti-inflammatory drugs (NSAIDs) which can irritate the stomach lining.
- Parasitic infections (e.g., hookworm) in some regions.
- Frequent Blood Donation: While generally safe, very frequent blood donation can, over time, lead to iron depletion and a transiently low hematocrit if iron stores are not adequately replenished.
- Urinary Tract Bleeding: Less common, but chronic bleeding from the kidneys or bladder can also contribute to blood loss.
The symptoms of chronic blood loss are often the same as those of iron-deficiency anemia: gradual onset of fatigue, weakness, pallor, and reduced exercise tolerance. Because the symptoms develop slowly, individuals may adapt to them, delaying diagnosis.
Other Causes of Low Hematocrit
While anemia and blood loss are the most common culprits, other factors can contribute to a low hematocrit:
- Overhydration (Dilutional Effect): An excessive amount of fluid in the bloodstream can dilute the concentration of red blood cells, leading to a falsely low hematocrit reading. This can occur with aggressive intravenous fluid administration or certain medical conditions that cause fluid retention.
- Bone Marrow Disorders: Beyond aplastic anemia, conditions like myelodysplastic syndromes, leukemias, or lymphomas can impair the bone marrow's ability to produce healthy red blood cells, resulting in low Hct.
- Kidney Disease: The kidneys produce erythropoietin (EPO), a hormone that stimulates red blood cell production in the bone marrow. Chronic kidney disease can lead to decreased EPO production, resulting in "anemia of chronic kidney disease" and a low hematocrit.
- Nutritional Deficiencies (beyond iron and B12/folate): Deficiencies in other nutrients like copper or vitamin C can also indirectly affect red blood cell production.
- Certain Medications: Some drugs, including chemotherapy agents, antibiotics, and certain anti-inflammatory medications, can suppress bone marrow function or cause red blood cell destruction.
- Hemolysis: The premature destruction of red blood cells, which can be caused by various factors including autoimmune diseases, infections, certain medications, or inherited disorders.
Symptoms of Low Hematocrit
The symptoms associated with low hematocrit are primarily due to the body's tissues and organs not receiving enough oxygen. These can range from mild to severe depending on the degree and rapidity of the Hct drop:
- Fatigue and Weakness: The most common symptoms, due to insufficient oxygen for energy production.
- Pallor: Pale skin, especially noticeable in the face, lips, and nail beds, as well as the conjunctiva of the eyes.
- Shortness of Breath (Dyspnea): Especially during physical activity, as the body struggles to meet oxygen demands.
- Dizziness or Lightheadedness: Due to reduced oxygen supply to the brain.
- Cold Hands and Feet: Impaired circulation and oxygen delivery to extremities.
- Headaches: Another symptom related to reduced oxygen to the brain.
- Chest Pain (Angina): In severe cases, especially in individuals with pre-existing heart conditions, the heart may struggle to compensate, leading to chest pain.
- Irregular Heartbeats (Tachycardia): The heart beats faster to try and pump more oxygenated blood.
- Brittle Nails and Hair Loss: More common in chronic iron-deficiency anemia.
- Pica: Cravings for non-food items like ice, dirt, or clay, sometimes seen in severe iron deficiency.
Diagnosis of Low Hematocrit and Underlying Causes
Diagnosing a low hematocrit begins with a routine complete blood count (CBC). If the CBC shows a low Hct (and typically low hemoglobin), further investigations are necessary to pinpoint the underlying cause.
Diagnostic steps may include:
- Red Blood Cell Indices: Part of the CBC, these provide information about the size and hemoglobin content of red blood cells (e.g., MCV, MCH, MCHC), helping to classify the type of anemia.
- Iron Studies: Tests such as serum iron, ferritin (iron storage protein), total iron-binding capacity (TIBC), and transferrin saturation help determine if iron deficiency is the cause.
- Vitamin B12 and Folate Levels: To check for deficiencies in these crucial vitamins.
- Stool Occult Blood Test: To detect hidden blood in the stool, indicating gastrointestinal bleeding.
- Endoscopy or Colonoscopy: If GI bleeding is suspected, these procedures allow direct visualization of the digestive tract.
- Kidney Function Tests: To assess kidney health and EPO production.
- Thyroid Function Tests: To rule out thyroid disorders that can sometimes cause anemia.
- Bone Marrow Biopsy: In cases of suspected bone marrow disorders or unexplained anemia.
- Genetic Testing: For inherited anemias like sickle cell disease or thalassemia.
- Evaluation for Hemolysis: Tests for red blood cell destruction if hemolytic anemia is suspected.
Treatment and Management
The treatment for low hematocrit is entirely dependent on its underlying cause. Addressing the root problem is paramount to restoring healthy red blood cell levels and alleviating symptoms.
- For Iron-Deficiency Anemia:
- Iron Supplementation: Oral iron tablets are typically prescribed. In severe cases or malabsorption, intravenous iron may be necessary.
- Dietary Changes: Increasing intake of iron-rich foods (red meat, poultry, fish, beans, fortified cereals, dark leafy greens) and foods high in vitamin C (which enhances iron absorption).
- Treating Blood Loss Source: Identifying and stopping the source of chronic blood loss (e.g., managing heavy menstrual bleeding, treating GI ulcers, removing polyps).
- For Vitamin Deficiency Anemias:
- Vitamin B12 Injections or Oral Supplements: Especially for pernicious anemia or severe dietary deficiency.
- Folate Supplements: Often prescribed with dietary adjustments.
- For Anemia of Chronic Disease:
- Managing the Underlying Chronic Condition: Treating the inflammatory disease, infection, or cancer is key.
- Erythropoiesis-Stimulating Agents (ESAs): In some cases, synthetic erythropoietin may be administered to stimulate red blood cell production, particularly in chronic kidney disease.
- For Aplastic Anemia and Other Bone Marrow Disorders:
- Immunosuppressive Therapy: To suppress the immune system if it's attacking bone marrow.
- Blood Transfusions: To temporarily increase red blood cell count.
- Bone Marrow Transplant: A potential curative option for severe cases.
- For Acute Blood Loss:
- Stopping the Bleeding: Immediate medical intervention to control the source of hemorrhage.
- Blood Transfusions: To rapidly replace lost blood volume and red blood cells.
- Intravenous Fluids: To restore overall blood volume.
Actionable Advice and When to See a Doctor
- Don't Self-Diagnose: If you experience persistent symptoms like fatigue, pallor, or shortness of breath, consult a healthcare provider. These symptoms can indicate a range of conditions, and accurate diagnosis is crucial.
- Regular Check-ups: Routine physical examinations and blood tests can help detect low hematocrit early, even before symptoms become severe.
- Balanced Diet: Ensure your diet is rich in iron, vitamin B12, and folate. If you follow a vegetarian or vegan diet, pay extra attention to sources of these nutrients and consider fortified foods or supplements under medical guidance.
- Monitor Menstrual Health: If you experience unusually heavy or prolonged menstrual periods, discuss this with your gynecologist.
- Beware of GI Symptoms: Any signs of blood in stool (black, tarry stools or bright red blood), persistent abdominal pain, or unexplained weight loss should prompt immediate medical evaluation.
- Medication Awareness: Discuss all medications, including over-the-counter drugs and supplements, with your doctor, as some can affect blood counts.
While this article focuses on low hematocrit, it's also important to be aware that hematocrit levels can be abnormally high. An elevated hematocrit, or polycythemia, also has significant health implications and requires medical attention, as detailed in our article on [high hematocrit causes and health implications].
In conclusion, a low hematocrit is a significant indicator that should never be ignored. It serves as a critical warning sign, often pointing to anemia or blood loss, both of which require prompt medical evaluation and treatment to prevent further complications and restore your health.
Frequently Asked Questions
What is the most common cause of abnormal Hematocrit (Hct) levels?
The most common cause of abnormally low Hematocrit (Hct) levels is iron-deficiency anemia, which itself is often a result of chronic blood loss (such as heavy menstrual periods or gastrointestinal bleeding) or inadequate dietary iron intake. For abnormally high Hct levels, dehydration is a very common cause, as it concentrates the red blood cells in a reduced plasma volume. However, other conditions like polycythemia vera can also cause pathologically high Hct.
How often should I get my Hematocrit (Hct) tested?
The frequency of Hematocrit (Hct) testing depends on your age, overall health, and any existing medical conditions. For healthy adults with no symptoms or known risk factors for anemia, Hct is typically tested as part of a routine complete blood count (CBC) during an annual physical exam, or every 3-5 years. If you have chronic conditions (like kidney disease, inflammatory bowel disease, or cancer), are pregnant, experience symptoms of anemia, or are undergoing treatment that affects blood cell production, your doctor may recommend more frequent testing, ranging from every few months to annually. Always follow your healthcare provider's specific recommendations.
Can lifestyle changes improve my Hematocrit (Hct) levels?
Yes, certain lifestyle changes can significantly improve Hematocrit (Hct) levels, especially when the low Hct is due to nutritional deficiencies or chronic mild blood loss.
- Dietary Adjustments: Increasing intake of iron-rich foods (red meat, poultry, fish, lentils, beans, spinach, fortified cereals), vitamin C (which aids iron absorption, found in citrus fruits, bell peppers), vitamin B12 (meat, dairy, fortified foods), and folate (leafy greens, legumes, fortified grains) can help the body produce healthy red blood cells.
- Addressing Blood Loss: If heavy menstrual bleeding is a cause, discussing management options with a gynecologist can help. For gastrointestinal blood loss, identifying and treating the underlying cause (e.g., dietary changes for ulcers, medication adjustments) is crucial.
- Hydration: Maintaining adequate hydration can prevent falsely elevated Hct readings due to dehydration, although it won't directly raise Hct if it's genuinely low.
- Avoiding Alcohol and Smoking: Excessive alcohol intake can interfere with nutrient absorption and bone marrow function, while smoking can lead to high Hct (polycythemia) due to chronic hypoxia rather than improving low Hct. These changes are most effective when guided by a healthcare professional, especially if the low Hct is due to underlying medical conditions.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.