Vitamin A Benefits for Vision and Skin Health
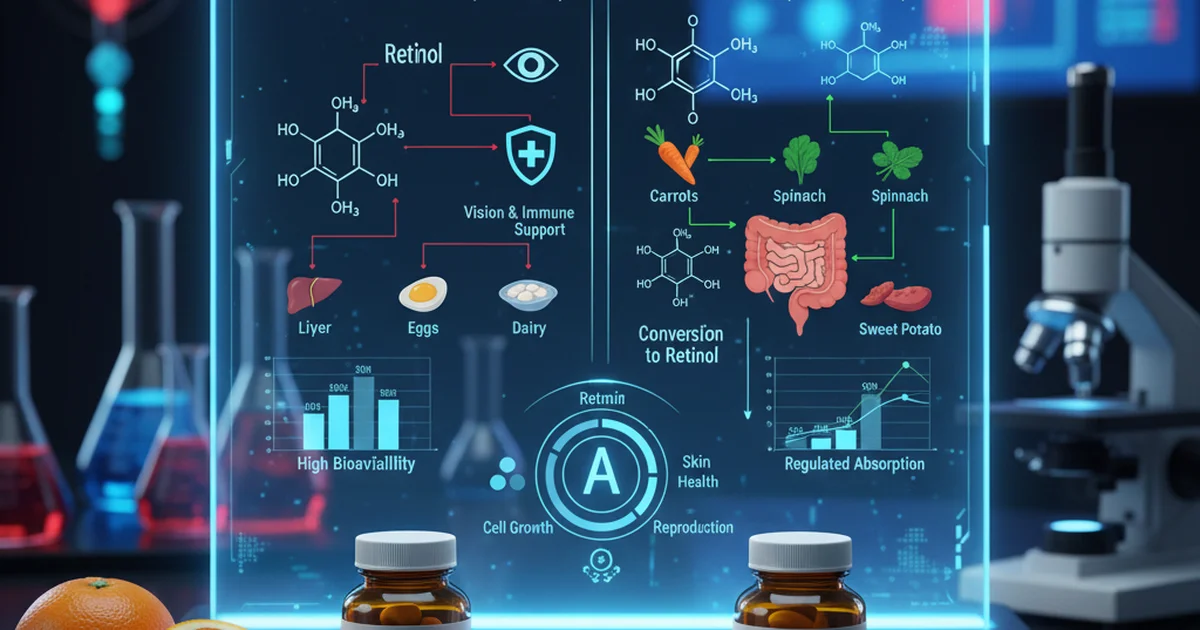
Vitamin A is an essential fat-soluble vitamin that plays a critical role in numerous physiological processes, most notably in maintaining healthy vision, robust immune function, and vibrant skin. It exists in two primary forms: preformed Vitamin A (retinoids), found in animal products, and provitamin A carotenoids, found in plant-based foods, which the body converts into Vitamin A. Understanding the nuances of its dietary sources, bioavailability, and the judicious use of supplementation is key to harnessing its powerful benefits while avoiding potential pitfalls.
The Dual Nature of Vitamin A: Retinoids and Carotenoids
Vitamin A is not a single compound but a group of unsaturated nutritional organic compounds that include retinol, retinal, retinoic acid, and several provitamin A carotenoids.
Preformed Vitamin A (Retinoids)
These are biologically active forms of Vitamin A, primarily found in animal-derived foods.
- Retinol: The alcohol form, often stored in the liver. It's the primary form transported in the blood.
- Retinal (Retinaldehyde): Crucial for vision.
- Retinoic Acid: Essential for gene expression, cell differentiation, and growth, playing a significant role in skin health and immune function.
Provitamin A Carotenoids
These are plant pigments that the body can convert into Vitamin A. The most common and potent provitamin A carotenoid is beta-carotene.
- Beta-carotene: Found abundantly in colorful fruits and vegetables. It's cleaved by an enzyme in the intestine (beta-carotene 15,15'-monooxygenase) to form two molecules of retinal.
- Other Carotenoids: Alpha-carotene and beta-cryptoxanthin are also provitamin A carotenoids, though less potent than beta-carotene.
Vitamin A's Indispensable Role in Vision
One of Vitamin A's most renowned functions is its critical involvement in maintaining healthy eyesight, particularly in low-light conditions.
The Phototransduction Cycle
- Rhodopsin Formation: In the retina of the eye, retinal (a form of Vitamin A) combines with the protein opsin to form rhodopsin. Rhodopsin is a light-sensitive pigment found in the rod cells, which are responsible for vision in dim light and detecting motion.
- Light Absorption: When light strikes rhodopsin, it causes a conformational change in the retinal molecule, triggering a cascade of biochemical events that send electrical signals to the brain, allowing us to perceive light.
- Regeneration: After detecting light, retinal detaches from opsin, and a portion is converted back to its original form to regenerate rhodopsin. This continuous cycle requires a steady supply of Vitamin A.
- Night Vision: A deficiency in Vitamin A directly impairs this cycle, leading to xerophthalmia, a progressive eye disease that begins with night blindness (nyctalopia) – difficulty seeing in low light. Without adequate Vitamin A, the regeneration of rhodopsin is hampered, making it harder for the eyes to adapt to darkness.
- Conjunctival and Corneal Health: Beyond its role in the retina, Vitamin A also maintains the health of the conjunctiva (the membrane lining the eyelids and covering the white part of the eye) and the cornea (the transparent outer layer of the eye). Deficiency can lead to dryness (xerosis), Bitot's spots (foamy patches on the conjunctiva), and in severe cases, corneal ulceration and permanent blindness.
Enhancing Skin Health and Integrity
Vitamin A, particularly in its retinoic acid form, is a powerhouse for skin health, influencing cell growth, differentiation, and repair.
Cell Differentiation and Turnover
- Epithelial Cell Growth: Retinoic acid is crucial for the normal growth and differentiation of epithelial cells, which form the outer layer of the skin (epidermis) and line various internal organs. It helps maintain the integrity and barrier function of the skin.
- Keratinization: Vitamin A regulates the process of keratinization, where skin cells produce keratin. Proper keratinization ensures a healthy skin barrier, preventing excessive water loss and protecting against environmental damage.
- Anti-Aging Properties: Retinoids, both topical and systemic, are widely used in dermatology for their anti-aging effects. They stimulate collagen production, reduce collagen degradation, and promote cell turnover, which helps to smooth fine lines and wrinkles, improve skin texture, and reduce hyperpigmentation.
- Acne Treatment: Retinoic acid derivatives (retinoids) are highly effective in treating acne. They work by:
- Reducing sebum production: Decreasing the activity of sebaceous glands.
- Preventing clogged pores: Normalizing the shedding of dead skin cells, preventing them from accumulating and blocking hair follicles.
- Anti-inflammatory effects: Reducing inflammation associated with acne lesions.
Dietary Sources: Fueling Your Body Naturally
Obtaining Vitamin A through diet is the safest and most effective way to ensure adequate intake. Dietary sources are categorized by whether they contain preformed Vitamin A or provitamin A carotenoids.
Sources of Preformed Vitamin A
These are readily absorbed and utilized by the body.
- Liver: Organ meats, particularly beef liver, are exceptionally rich sources of Vitamin A. A small serving can provide several times the recommended daily intake.
- Fish Liver Oils: Cod liver oil is a well-known supplement rich in Vitamin A and Vitamin D.
- Dairy Products: Milk, cheese, and butter are good sources, often fortified with Vitamin A.
- Eggs: Egg yolks contain a moderate amount of Vitamin A.
- Fortified Foods: Many cereals, margarines, and other processed foods are fortified with Vitamin A.
Sources of Provitamin A Carotenoids
These need to be converted by the body, and their absorption can be influenced by several factors.
- Orange and Yellow Vegetables: Carrots, sweet potatoes, pumpkin, butternut squash, and bell peppers are excellent sources of beta-carotene.
- Dark Green Leafy Vegetables: Spinach, kale, collard greens, and broccoli also contain significant amounts of beta-carotene, though the green chlorophyll pigment often masks the orange color.
- Orange Fruits: Cantaloupe, apricots, and mangoes are rich in provitamin A carotenoids.
Bioavailability and Conversion Efficiency
The amount of Vitamin A your body actually absorbs and utilizes from food can vary significantly. This concept is known as bioavailability.
Factors Affecting Bioavailability
- Fat Intake: Since Vitamin A is fat-soluble, its absorption from the digestive tract is significantly enhanced when consumed with dietary fat. A meal containing healthy fats (e.g., olive oil, avocado, nuts) will improve the absorption of both preformed Vitamin A and carotenoids.
- Food Matrix: The way food is prepared can affect bioavailability.
- Cooking: Light cooking (e.g., steaming, sautéing) can break down cell walls in plant foods, making carotenoids more accessible for absorption, but overcooking can destroy some nutrients.
- Pureeing/Mashing: Processing plant foods (e.g., carrot juice, sweet potato puree) can also increase the bioavailability of carotenoids.
- Individual Conversion Efficiency: The conversion of provitamin A carotenoids (like beta-carotene) into Vitamin A is not 100% efficient and varies greatly among individuals.
- Genetics: Genetic variations can influence the activity of the enzyme beta-carotene 15,15'-monooxygenase.
- Nutritional Status: Conditions like zinc deficiency can impair the conversion of beta-carotene to Vitamin A and the transport of Vitamin A from the liver. Iron deficiency can also affect the conversion.
- Health Conditions: Certain medical conditions affecting fat absorption (e.g., celiac disease, Crohn's disease, pancreatic insufficiency, liver disease) can significantly reduce Vitamin A absorption.
Due to varying conversion rates, the concept of Retinol Activity Equivalents (RAE) was developed to standardize Vitamin A intake.
- 1 RAE = 1 mcg retinol
- 1 RAE = 12 mcg beta-carotene from food
- 1 RAE = 2 mcg supplemental beta-carotene
- 1 RAE = 24 mcg other provitamin A carotenoids from food This highlights that you need much more beta-carotene from food to get the same Vitamin A activity as preformed retinol.
Supplementation: When and How
While a balanced diet is usually sufficient, supplementation may be necessary for individuals with specific needs or deficiencies.
Who Might Benefit from Supplementation?
- Individuals with Malabsorption Issues: People with conditions like cystic fibrosis, celiac disease, Crohn's disease, or chronic pancreatitis may struggle to absorb fat-soluble vitamins, including Vitamin A.
- Those with Chronic Liver Disease: The liver is crucial for Vitamin A storage and metabolism.
- Individuals with Severe Dietary Restrictions: Vegans or those with very limited diets might need to pay close attention to their provitamin A intake or consider supplementation if dietary sources are insufficient.
- Diagnosed Deficiency: If blood tests reveal a deficiency, supplementation under medical guidance is essential. You can learn more about identifying low levels and their implications in our article on [Vitamin A normal range and deficiency signs].
Types of Vitamin A Supplements
- Retinyl Palmitate or Retinyl Acetate: These are common forms of preformed Vitamin A found in supplements, often derived from fish liver oil.
- Beta-carotene: Supplements containing beta-carotene are also available. These are generally considered safer in high doses than preformed Vitamin A because the body only converts what it needs, reducing the risk of toxicity. However, high doses of beta-carotene supplements are not recommended for smokers due to potential increased lung cancer risk.
Dosage and Safety
- Recommended Daily Allowance (RDA):
- Adult men: 900 mcg RAE (3000 IU)
- Adult women: 700 mcg RAE (2333 IU)
- These values are for preventing deficiency.
- Tolerable Upper Intake Level (UL): The UL for preformed Vitamin A is 3,000 mcg RAE (10,000 IU) per day for adults. Exceeding this limit consistently can lead to toxicity, as Vitamin A is fat-soluble and can accumulate in the body.
- Consult a Healthcare Professional: It is crucial to consult a doctor or registered dietitian before starting Vitamin A supplementation, especially for high doses or if you are pregnant or breastfeeding. Excessive intake of preformed Vitamin A during pregnancy can cause birth defects.
Potential Risks: Hypervitaminosis A
While essential, Vitamin A is not without its risks, particularly when consumed in excess through supplements. Unlike water-soluble vitamins, fat-soluble vitamins like A are stored in the body, primarily in the liver, and can accumulate to toxic levels.
Acute vs. Chronic Toxicity
- Acute Toxicity: Occurs from a single, very large dose (e.g., consuming polar bear liver). Symptoms include nausea, vomiting, headache, dizziness, blurred vision, and muscle incoordination.
- Chronic Toxicity (Hypervitaminosis A): Develops from consistently exceeding the UL over time. Symptoms can be wide-ranging and include:
- Skin changes: Dry, rough skin, hair loss, peeling, itching.
- Neurological symptoms: Severe headaches, dizziness, blurred vision, bulging fontanelles in infants (pseudotumor cerebri).
- Liver damage: Enlarged liver, abnormal liver function tests, cirrhosis.
- Bone and joint pain: Increased risk of fractures, bone demineralization.
- Birth defects: Teratogenic effects if high doses are taken during pregnancy.
It is vital to be aware of these risks. For a comprehensive understanding of the signs and symptoms of too much Vitamin A, refer to our detailed article on [Hypervitaminosis A symptoms of Vitamin A toxicity].
Vitamin A Reference Ranges
Monitoring Vitamin A levels, particularly for individuals at risk of deficiency or toxicity, is important. Serum retinol is the primary indicator of Vitamin A status.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 20-60 | mcg/dL | Varies by lab, generally consistent |
| Adult Women | 20-60 | mcg/dL | May be slightly lower during pregnancy |
| Children (1-10 years) | 15-50 | mcg/dL | Age-dependent, generally lower in younger children |
| Infants (0-1 year) | 10-30 | mcg/dL | Lower than adults, rapidly increases post-birth |
Note: These ranges are general guidelines and can vary slightly depending on the laboratory and the specific assay used. Always interpret results in consultation with a healthcare professional.
Actionable Advice for Optimal Vitamin A Intake
- Embrace a Colorful Diet: Prioritize a wide variety of fruits and vegetables, especially those that are orange, yellow, and dark green. These provide provitamin A carotenoids along with other beneficial nutrients and antioxidants.
- Include Healthy Fats: Always consume provitamin A-rich foods with a source of healthy fats (e.g., olive oil dressing on salads, avocado with carrots) to maximize absorption.
- Moderate Animal Sources: If you consume animal products, incorporate liver occasionally and ensure regular intake of dairy and eggs to provide preformed Vitamin A.
- Cooking Matters: Lightly cook vegetables like carrots and spinach to enhance beta-carotene bioavailability, but avoid overcooking which can degrade nutrients.
- Supplement Wisely: If you suspect a deficiency or have malabsorption issues, consult your doctor. If supplementation is recommended, stick to the prescribed dosage and be mindful of the Tolerable Upper Intake Level, especially for preformed Vitamin A.
- Avoid Excessive Doses: Never exceed the recommended daily allowance or the UL for Vitamin A supplements without strict medical supervision, particularly if you are pregnant or planning pregnancy.
In conclusion, Vitamin A is a vital nutrient with profound impacts on vision and skin health. By focusing on a diverse, nutrient-rich diet and understanding the factors that influence its absorption and utilization, individuals can effectively support their health. When considering supplementation, a cautious, informed approach guided by medical expertise is paramount to reap the benefits while mitigating the risks of deficiency and toxicity.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin A levels?
The most common cause of abnormal Vitamin A levels is dietary inadequacy or excess. Globally, Vitamin A deficiency is a significant public health problem, particularly in developing countries, often due to insufficient intake of Vitamin A-rich foods. On the other hand, in developed countries, abnormal levels are more often linked to excessive supplementation with preformed Vitamin A, leading to toxicity. Malabsorption syndromes (e.g., celiac disease, Crohn's disease, pancreatic insufficiency) or chronic liver disease can also lead to deficiency, while certain medical conditions or very high intake of specific organ meats (like polar bear liver) can cause acute toxicity.
How often should I get my Vitamin A tested?
Routine Vitamin A testing is generally not recommended for healthy individuals who consume a balanced diet. Testing is typically reserved for those with specific risk factors or symptoms. You might consider testing if you:
- Have symptoms of Vitamin A deficiency (e.g., night blindness, dry eyes, poor immune function, skin issues).
- Have symptoms suggestive of Vitamin A toxicity (e.g., severe headaches, hair loss, dry skin, bone pain).
- Suffer from conditions that impair fat absorption (e.g., cystic fibrosis, celiac disease, Crohn's disease, chronic pancreatitis).
- Have chronic liver disease.
- Are undergoing bariatric surgery.
- Are pregnant or planning pregnancy and have concerns about intake or exposure.
- Are taking high-dose Vitamin A supplements. Your healthcare provider will determine the appropriate frequency based on your individual health status and risk factors.
Can lifestyle changes improve my Vitamin A levels?
Absolutely, significant improvements in Vitamin A levels can be achieved through lifestyle changes, primarily focusing on dietary adjustments.
- Dietary Diversity: Incorporate a wide array of Vitamin A-rich foods. This means regularly consuming orange and yellow fruits and vegetables (carrots, sweet potatoes, mangoes), dark leafy greens (spinach, kale), and moderate amounts of animal sources like liver, eggs, and dairy if applicable to your diet.
- Fat Intake with Meals: Always pair provitamin A carotenoid-rich plant foods with a source of healthy fats (e.g., olive oil, avocado, nuts, seeds) to enhance absorption.
- Proper Food Preparation: Lightly cooking vegetables can help break down cell walls, making carotenoids more bioavailable.
- Address Underlying Conditions: If you have a condition affecting nutrient absorption, working with a healthcare provider to manage that condition can indirectly improve your Vitamin A status.
- Avoid Excessive Alcohol: Chronic alcohol consumption can impair liver function and Vitamin A metabolism, so moderation is key. These changes can help optimize your body's absorption, conversion, and utilization of Vitamin A from dietary sources.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.