Symptoms of Vitamin D Deficiency You Shouldn't Ignore
Vitamin D, specifically the circulating form 25‑hydroxyvitamin D [25(OH)D], is essential for bone health, immune regulation, and many metabolic processes. While many people assume that a “sunny” climate guarantees adequate levels, modern indoor lifestyles, sunscreen use, and dietary patterns frequently lead to suboptimal status. Ignoring early signs of deficiency can set the stage for chronic disease, fractures, and impaired quality of life. This article explores the clinical clues that merit attention, the science behind dietary sources and bioavailability, and practical strategies for testing and supplementation.
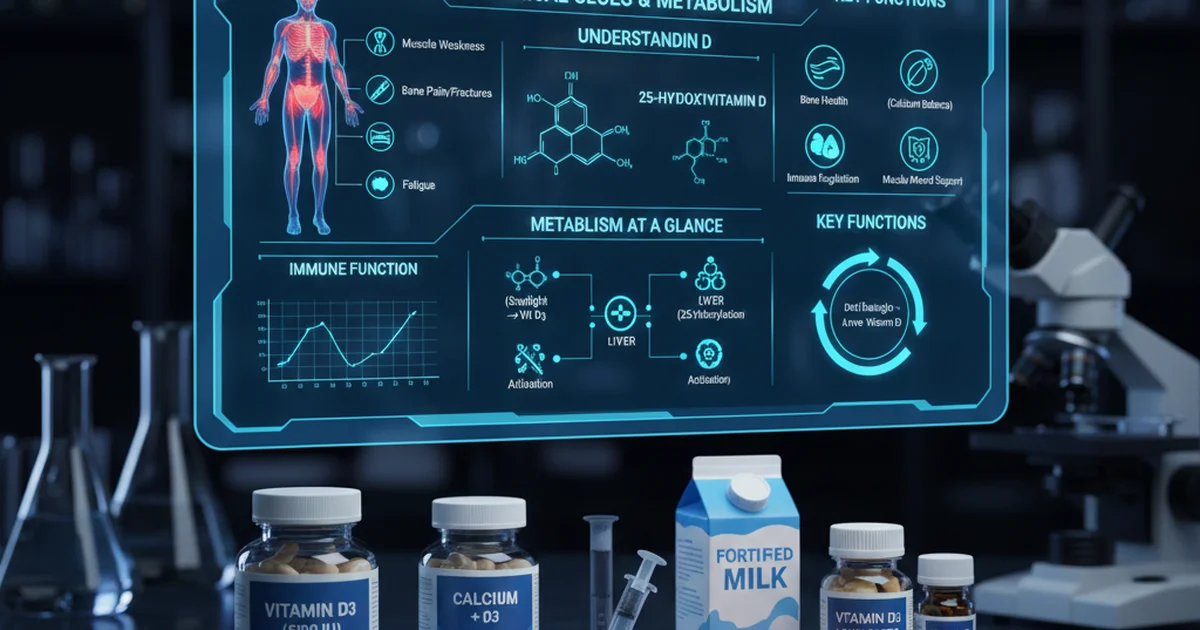
Understanding 25‑Hydroxyvitamin D
- What it is: 25(OH)D is the major circulating metabolite of vitamin D and the best indicator of overall vitamin D stores. It reflects intake from food, supplements, and cutaneous synthesis.
- Why it matters: Once converted to the active hormone 1,25‑dihydroxyvitamin D in the kidneys, it regulates calcium‑phosphate balance, modulates innate and adaptive immunity, influences muscle function, and even affects mood and cardiovascular health.
- Metabolism at a glance:
- Skin – UVB photons convert 7‑dehydrocholesterol to pre‑vitamin D₃, which thermally isomerizes to vitamin D₃.
- Liver – Vitamin D₃ (or D₂ from plant sources) is hydroxylated to 25(OH)D.
- Kidney – 25(OH)D is further hydroxylated to the active 1,25‑(OH)₂D.
Reference Ranges for Serum 25‑Hydroxyvitamin D
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adults (≥19 y) – General | 30–100 | ng/mL | ≥30 ng/mL considered sufficient by most societies |
| Adults – High‑risk (osteoporosis, malabsorption) | 40–100 | ng/mL | Higher target to protect bone health |
| Children (0‑18 y) | 20–100 | ng/mL | Infants may need 30–50 ng/mL for optimal growth |
| Pregnant & Lactating Women | 30–100 | ng/mL | Adequate levels support fetal skeletal development |
| Elderly (>65 y) | 30–100 | ng/mL | Deficiency linked to falls and fractures |
| Dark‑skinned populations | 30–100 | ng/mL | May require higher sun exposure or supplementation |
Values below 20 ng/mL are widely accepted as deficient; 20‑29 ng/mL is considered insufficient.
Clinical Symptoms You Shouldn't Ignore
Vitamin D deficiency often masquerades as vague or unrelated complaints. Recognizing the pattern early can prompt testing and treatment before irreversible damage occurs.
1. Musculoskeletal Complaints
- Bone pain (especially in the ribs, pelvis, or long bones)
- Diffuse muscle weakness that worsens with activity
- Frequent falls in older adults – low vitamin D impairs neuromuscular coordination
2. Fatigue & General Malaise
- Persistent low‑energy states not explained by sleep or psychiatric causes
- “Brain fog” – difficulty concentrating, short‑term memory lapses
3. Immune‑Related Issues
- Recurrent upper‑respiratory infections or prolonged viral illnesses
- Autoimmune flare‑ups (e.g., psoriasis, rheumatoid arthritis) may correlate with low levels
4. Mood Disturbances
- Depressive symptoms especially in winter months or in individuals with limited sun exposure
- Seasonal affective patterns that improve with vitamin D repletion
5. Metabolic Signals
- Insulin resistance and unexplained weight gain
- Elevated parathyroid hormone (PTH) secondary to low calcium absorption
6. Dermatologic Clues
- Hair thinning or alopecia areata has been linked to inadequate vitamin D status
When any of these signs persist despite conventional management, consider checking serum 25(OH)D.
Dietary Sources of Vitamin D
Unlike many vitamins, few foods naturally contain significant vitamin D. Understanding the options helps patients optimize intake, especially when sunlight is limited.
| Food Category | Typical Vitamin D Content (IU per serving) | Bioavailability Notes |
|---|---|---|
| Fatty fish (salmon, mackerel, sardines) | 400–600 | Highly bioavailable; omega‑3 fats aid absorption |
| Cod liver oil | 450–1,000 | Concentrated source; also provides vitamin A and K₂ |
| Egg yolk (from chickens raised outdoors) | 40–50 | Dependent on hen diet; modest contribution |
| Fortified dairy (milk, yogurt) | 100–150 | Vitamin D added in a water‑soluble form; calcium enhances uptake |
| Fortified plant milks (soy, almond) | 100–150 | Similar to dairy; check for vitamin D₃ vs D₂ |
| UV‑exposed mushrooms (e.g., maitake) | 200–400 | Naturally produce vitamin D₂; less potent than D₃ |
| Beef liver | 40–50 | Small amount; not a primary source |
Key point: Vitamin D₃ (cholecalciferol) is more effective at raising serum 25(OH)D than vitamin D₂ (ergocalciferol). Whenever possible, prioritize D₃ sources or supplements.
Bioavailability: How the Body Handles Vitamin D
- Fat‑soluble nature: Vitamin D requires dietary fat for optimal absorption. Consuming it with a meal containing 5–10 g of fat improves uptake by up to 30 %.
- Intestinal transport: After emulsification by bile salts, vitamin D is incorporated into micelles and taken up by enterocytes.
- Genetic factors: Polymorphisms in the GC gene (vitamin D‑binding protein) and CYP2R1 (hepatic 25‑hydroxylase) can affect serum levels despite similar intake.
- Age‑related decline: Elderly skin produces ~25 % less vitamin D₃ per UVB exposure; intestinal absorption may also be reduced.
Supplementation Strategies
When diet and sunlight are insufficient, supplementation becomes the cornerstone of correction.
Choosing the Right Form
- Vitamin D₃ (cholecalciferol) – Preferred for most adults; raises serum 25(OH)D more reliably.
- Vitamin D₂ (ergocalciferol) – Useful for vegans; may require higher doses to achieve the same serum rise.
Dosage Guidelines (based on baseline status)
| Baseline 25(OH)D | Goal | Typical Daily Dose | Typical Weekly Dose |
|---|---|---|---|
| <10 ng/mL (severe) | ≥30 ng/mL | 4,000–10,000 IU | 30,000–70,000 IU |
| 10–19 ng/mL (deficient) | ≥30 ng/mL | 2,000–4,000 IU | 15,000–30,000 IU |
| 20–29 ng/mL (insufficient) | ≥30 ng/mL | 1,000–2,000 IU | 7,000–15,000 IU |
| ≥30 ng/mL (sufficient) | Maintain | 600–1,000 IU (RDA) | 4,200–7,000 IU |
Higher doses may be needed for obesity, malabsorption, or certain medications (e.g., glucocorticoids, anticonvulsants).
Safety Considerations
- Upper intake level for adults is generally 4,000 IU/day; short‑term higher doses are safe under medical supervision.
- Hypercalcemia is rare but can occur with chronic intakes >10,000 IU/day, especially in patients with granulomatous diseases or sarcoidosis.
- Kidney stones: Adequate hydration mitigates risk; monitor calcium excretion if using very high doses.
Practical Tips for Patients
- Take with food containing fat (e.g., a glass of milk, a handful of nuts).
- Consistency matters: Daily dosing yields steadier serum levels than intermittent mega‑doses for most individuals.
- Combine with calcium (1,000–1,200 mg/day) if bone health is a primary concern, but avoid excessive calcium supplementation without medical guidance.
Testing Frequency and Interpretation
- Initial assessment: Baseline serum 25(OH)D when symptoms arise or before initiating high‑dose therapy.
- Re‑check: 8–12 weeks after starting supplementation to verify response; adjust dose accordingly.
- Maintenance monitoring: Annually for individuals on long‑term high‑dose regimens, those with chronic kidney disease, malabsorption syndromes, or on medications affecting vitamin D metabolism.
Interpretation nuances
- Seasonal variation: Levels often dip in winter; a slight decrease may be normal if still above 20 ng/mL.
- Laboratory differences: Some assays report in nmol/L (multiply by 0.4 to convert to ng/mL).
Who Is at Greatest Risk?
- Older adults – reduced skin synthesis and dietary intake.
- People with darker skin – melanin decreases UVB penetration.
- Individuals living at high latitudes – limited UVB during winter months.
- Obese persons – vitamin D is sequestered in adipose tissue, lowering circulating levels.
- Patients with malabsorption (celiac disease, Crohn’s disease, bariatric surgery).
- Those on certain medications (antiepileptics, glucocorticoids, antifungals).
Targeted screening in these groups can catch deficiency before complications develop.
Actionable Steps for Clinicians and Patients
- Screen high‑risk individuals annually or when musculoskeletal, immune, or mood symptoms emerge.
- Encourage safe sun exposure: 10–30 minutes of midday sun (face, arms, legs) 2–3 times per week, depending on skin type and season.
- Optimize diet: Prioritize fatty fish, fortified dairy or plant milks, and consider UV‑treated mushrooms for vegetarians.
- Prescribe supplementation based on baseline levels, body weight, and comorbidities; use vitamin D₃ whenever possible.
- Monitor: Reassess serum 25(OH)D after 8–12 weeks; adjust dose to maintain ≥30 ng/mL.
- Educate: Explain that “feeling fine” does not guarantee adequacy; many deficiencies are silent until a fracture or infection occurs.
- Address adherence barriers: Offer once‑weekly or monthly high‑dose formulations for patients who struggle with daily pills.
Bottom Line
Vitamin D deficiency presents with subtle yet clinically meaningful symptoms that span bone health, immunity, mood, and metabolism. Recognizing the early warning signs, understanding the limited dietary sources, and employing evidence‑based supplementation can prevent serious sequelae. Regular testing, especially in at‑risk populations, ensures that serum 25‑hydroxyvitamin D remains within the optimal range, supporting overall health and well‑being.
Frequently Asked Questions
What is the most common cause of abnormal Vitamin D (25-Hydroxy) levels?
The leading cause of low 25‑hydroxyvitamin D is inadequate sunlight exposure, often compounded by indoor occupations, high‑latitude living, extensive sunscreen use, or clothing that limits skin exposure. Dietary insufficiency and obesity are also frequent contributors, while certain medications and malabsorption disorders can further depress levels.
How often should I get my Vitamin D (25-Hydroxy) tested?
For most adults, an initial test followed by a repeat after 8–12 weeks of supplementation is sufficient to confirm adequacy. After achieving a stable, sufficient level, annual testing is recommended for high‑risk groups (elderly, obese, chronic kidney disease, malabsorption, or those on medications that affect vitamin D metabolism). Individuals with stable, sufficient levels and no risk factors may test every 2–3 years.
Can lifestyle changes improve my Vitamin D (25-Hydroxy) levels?
Absolutely. Regular, moderate sun exposure (10–30 minutes of midday UVB several times per week) is the most natural way to boost synthesis. Pairing vitamin D‑rich foods—such as fatty fish, fortified dairy or plant milks, and UV‑treated mushrooms—with meals that contain healthy fats enhances absorption. Maintaining a healthy body weight and addressing any gastrointestinal issues that impair nutrient uptake also support optimal vitamin D status.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.