Low Transferrin Saturation: Anemia Links
Low Transferrin Saturation: Anemia Links
Reference Ranges for Transferrin Saturation
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adult Men | 20‑45 | % | Slightly higher on average; influenced by iron intake |
| Adult Women (premenopausal) | 15‑35 | % | Menstrual losses often lower the upper limit |
| Adult Women (post‑menopausal) | 20‑45 | % | Values converge with male range after menopause |
| Children (1‑12 yr) | 15‑35 | % | Age‑dependent; infants have higher physiological needs |
| Adolescents (13‑18 yr) | 15‑40 | % | Rapid growth and puberty affect iron demand |
| Pregnant Women | 15‑30 | % | Hemodilution and fetal iron transfer lower the upper limit |
| Elderly (>65 yr) | 20‑45 | % | Chronic disease may affect interpretation |
Introduction
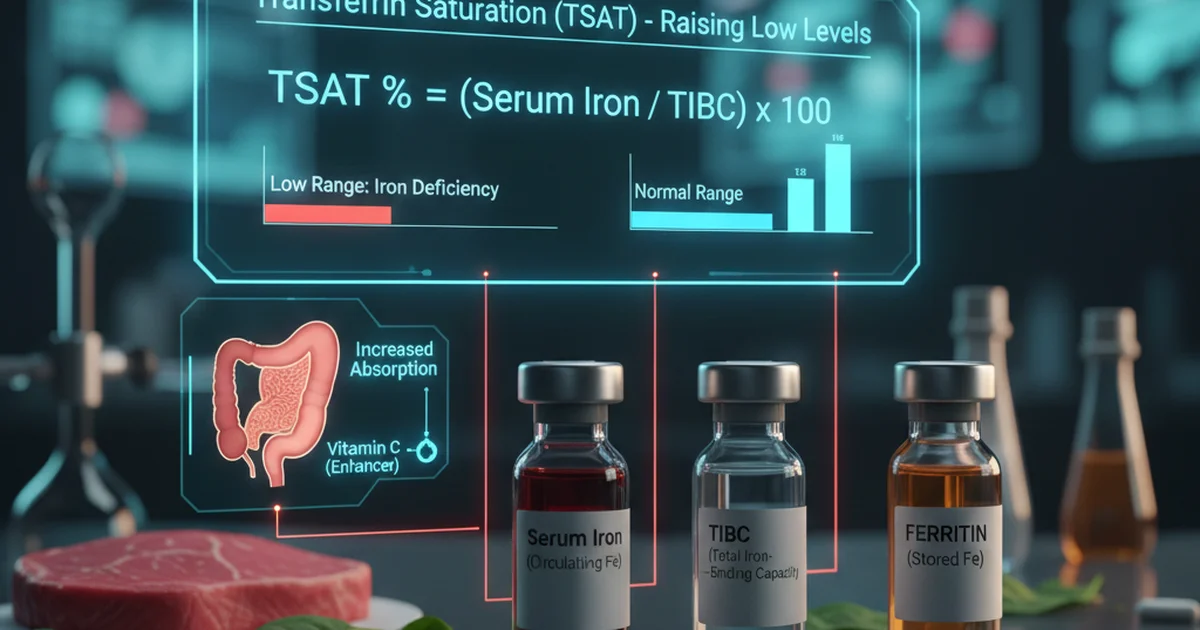
Transferrin saturation (TSAT) is a calculated laboratory value that reflects the proportion of transferrin—a plasma protein that transports iron—occupied by iron. It is derived from serum iron divided by total iron‑binding capacity (TIBC) and expressed as a percentage. Low TSAT is a hallmark of iron‑deficiency anemia (IDA) but can also signal chronic inflammation, malabsorption, or dietary insufficiency. Understanding the dietary sources, bioavailability, and appropriate supplementation strategies for raising TSAT is essential for clinicians, dietitians, and anyone seeking to prevent or treat anemia.
Physiology Overview
- Transferrin binds two ferric (Fe³⁺) ions per molecule; the amount of transferrin in plasma is reflected by TIBC.
- Serum iron measures the iron currently bound to transferrin.
- TSAT = (Serum Iron ÷ TIBC) × 100.
- Normal TSAT indicates a balance between iron intake, absorption, storage, and utilization.
- Low TSAT (< 15 %) suggests that the majority of transferrin is unoccupied, signaling a deficit in readily available iron for erythropoiesis.
Why Low TSAT Matters
- Erythropoiesis: Red blood cell production requires iron for hemoglobin synthesis. Insufficient iron leads to microcytic, hypochromic anemia.
- Cellular Metabolism: Iron is a cofactor for enzymes involved in oxidative phosphorylation and DNA synthesis; low availability can cause fatigue, impaired cognition, and reduced immune competence.
- Diagnostic Clue: TSAT is more sensitive than serum ferritin alone in distinguishing iron‑deficiency anemia from anemia of chronic disease, because ferritin is an acute‑phase reactant.
Dietary Sources of Iron
Heme Iron (Highly Bioavailable)
| Food | Approx. Iron Content (mg/100 g) |
|---|---|
| Beef liver | 6.5 |
| Chicken liver | 5.0 |
| Lean beef (steak) | 2.6 |
| Lamb | 2.0 |
| Pork | 1.2 |
| Turkey (dark meat) | 1.5 |
| Fish (salmon, tuna) | 0.8‑1.0 |
- Bioavailability: 15‑35 % of heme iron is absorbed, largely independent of other dietary factors.
- Practical tip: Include a modest portion (≈ 100 g) of heme‑rich meat or organ meat 2–3 times per week to support TSAT.
Non‑Heme Iron (Variable Bioavailability)
| Food | Approx. Iron Content (mg/100 g) |
|---|---|
| Lentils (cooked) | 3.3 |
| Chickpeas (cooked) | 2.9 |
| White beans (cooked) | 3.7 |
| Tofu (firm) | 2.7 |
| Spinach (cooked) | 3.6 |
| Swiss chard (cooked) | 2.0 |
| Pumpkin seeds | 8.8 |
| Quinoa (cooked) | 1.5 |
| Fortified breakfast cereals | 5‑20 (depends on brand) |
- Bioavailability: 2‑20 %, heavily influenced by enhancers (vitamin C, meat factor) and inhibitors (phytates, polyphenols, calcium).
- Enhancement strategies:
- Pair non‑heme iron foods with vitamin C‑rich items (citrus, berries, bell peppers).
- Combine with a small amount of meat, fish, or poultry (“meat factor”) to boost absorption up to 3‑fold.
- Inhibition mitigation:
- Soak, sprout, or ferment legumes and grains to reduce phytate content.
- Limit tea/coffee consumption within 1 hour of iron‑rich meals.
Factors Affecting Iron Bioavailability
| Factor | Effect on Absorption | Practical Guidance |
|---|---|---|
| Vitamin C | Increases non‑heme iron absorption by reducing Fe³⁺ to Fe²⁺ | Add citrus juice or raw peppers to meals |
| Meat factor | Enhances both heme and non‑heme iron uptake | Include ≤ 30 g of meat, fish, or poultry with plant‑based meals |
| Phytates (found in whole grains, legumes, nuts) | Chelate iron, lowering absorption | Use soaking/fermentation; consume fortified cereals |
| Polyphenols (tea, coffee, red wine) | Inhibit iron uptake | Avoid drinking these beverages with iron‑rich meals |
| Calcium (dairy, supplements) | Competes with iron for transporters | Separate calcium‑rich foods/supplements by ≥ 2 hours |
| Gastric acidity | Low acidity impairs Fe³⁺ reduction | Consider acid‑enhancing foods or a low‑dose HCl supplement if hypochlorhydria is present |
| Inflammation (hepcidin elevation) | Blocks iron export from enterocytes | Address underlying inflammatory conditions; TSAT may remain low despite adequate intake |
Clinical Evaluation of Low TSAT
- Confirm the laboratory value – repeat TSAT if borderline (< 15 %).
- Assess iron stores – serum ferritin, soluble transferrin receptor, and reticulocyte hemoglobin content provide complementary data.
- Identify underlying causes – dietary insufficiency, chronic blood loss (e.g., menorrhagia, gastrointestinal bleeding), malabsorption (celiac disease, bariatric surgery), or inflammation.
- Rule out confounders – acute infection can elevate ferritin and mask iron deficiency; TSAT is less affected but still requires context.
Dietary Management to Raise TSAT
Step‑by‑Step Meal Planning
- Breakfast – Fortified cereal (≈ 10 mg iron) + orange slices (vitamin C).
- Mid‑morning snack – Handful of pumpkin seeds + a small kiwi.
- Lunch – Lentil soup with sautéed spinach, topped with a drizzle of lemon juice; side of grilled chicken breast (≈ 30 g).
- Afternoon snack – Apple with a tablespoon of almond butter (moderate calcium, keep timing separate from iron‑rich meals).
- Dinner – Pan‑seared salmon (heme iron) with quinoa pilaf (non‑heme iron) and roasted red peppers (vitamin C).
- Evening – Herbal tea (avoid black tea) and a small piece of dark chocolate (iron source, polyphenol content modest).
- Timing tip: Keep calcium‑rich foods (dairy, fortified plant milks) at least two hours apart from iron‑rich meals.
- Hydration: Adequate water supports gastrointestinal transit and nutrient absorption.
Special Populations
- Pregnant women: Aim for 27 mg of elemental iron daily; include prenatal multivitamins with iron, plus iron‑rich meals.
- Vegetarians/Vegans: Emphasize fortified foods, legumes, seeds, and vitamin C pairing; consider a low‑dose iron supplement if TSAT remains < 15 % after dietary optimization.
- Elderly: Monitor for reduced gastric acidity; a mild acid‑stimulating agent (e.g., apple cider vinegar diluted) before iron meals may improve absorption.
Supplementation Strategies
When to Supplement
- Documented iron‑deficiency anemia (Hb < 12 g/dL in women, < 13 g/dL in men) and TSAT < 15 % despite dietary counseling.
- High‑risk situations: Chronic blood loss, pregnancy, pre‑operative preparation, or malabsorption syndromes.
Choice of Iron Form
| Form | Elemental Iron (mg per 100 mg) | Absorption Rate | Gastro‑intestinal Tolerability |
|---|---|---|---|
| Ferrous sulfate | 20 | High | Commonly causes constipation/epigastric discomfort |
| Ferrous gluconate | 12 | Moderate | Better tolerated; larger tablet size |
| Ferrous fumarate | 33 | High | Similar tolerability to sulfate |
| Heme iron polypeptide | 12‑14 | Very high (≈ 30 %) | Minimal GI side effects |
| Iron bisglycinate (chelated) | 20‑25 | Moderate‑high | Good tolerance, less interaction with food |
- Evidence‑based recommendation: Start with ferrous sulfate 325 mg (≈ 65 mg elemental iron) once daily if tolerable; split dosing (e.g., 325 mg every other day) may improve absorption when hepcidin spikes after each dose.
- Alternative: For patients with significant GI upset, switch to iron bisglycinate or heme iron polypeptide, which have comparable efficacy with fewer side effects.
Administration Tips
- Empty‑stomach: Take iron 1 hour before or 2 hours after meals for maximal absorption.
- Vitamin C boost: Consume a glass of orange juice or a vitamin C tablet with the dose.
- Avoid inhibitors: Do not take with calcium supplements, antacids, or tea/coffee.
- Duration: Continue therapy for 3‑6 months after normalization of hemoglobin and TSAT to replenish iron stores.
- Monitoring: Re‑check TSAT and ferritin after 4–6 weeks; adjust dose if TSAT remains < 15 % or if side effects arise.
Safety Considerations
- Iron overload: Rare in individuals without hereditary hemochromatosis; avoid high‑dose supplementation (> 200 mg elemental iron daily) unless medically indicated.
- Interactions: Iron chelates tetracyclines, quinolones, and levothyroxine; separate dosing by ≥ 2 hours.
- Pediatric dosing: Use weight‑based formulations (≈ 3 mg/kg elemental iron per day) and monitor growth parameters.
Lifestyle Factors That Influence TSAT
- Regular physical activity improves erythropoiesis and can modestly increase iron utilization efficiency.
- Adequate sleep supports hormonal regulation of hepcidin, the master iron‑regulatory hormone; chronic sleep deprivation may elevate hepcidin and lower TSAT.
- Stress management: Chronic stress can increase inflammatory cytokines, raising hepcidin levels and reducing iron absorption. Mind‑body practices (yoga, meditation) may indirectly benefit TSAT.
- Alcohol moderation: Excessive alcohol impairs liver function and can disrupt iron metabolism; limit intake to ≤ 1 drink/day for women, ≤ 2 drinks/day for men.
Putting It All Together: A Practical Action Plan
- Screen: Obtain TSAT, serum iron, TIBC, and ferritin.
- Identify cause: Review diet, menstrual history, gastrointestinal symptoms, and chronic disease status.
- Dietary optimization: Implement iron‑rich meals with vitamin C pairing; separate calcium and polyphenol intake.
- Supplement if needed: Choose appropriate iron formulation, dose, and timing; add vitamin C for enhanced absorption.
- Re‑evaluate: Check TSAT and hemoglobin after 4–6 weeks; adjust therapy accordingly.
- Maintain: Once TSAT is within normal range, continue a balanced diet and periodic monitoring (every 6–12 months) to prevent recurrence.
Frequently Asked Questions
What is the most common cause of abnormal Transferrin Saturation levels?
The most frequent cause of a low TSAT is iron‑deficiency anemia, typically resulting from inadequate dietary iron intake, chronic blood loss (e.g., heavy menstrual periods, gastrointestinal bleeding), or increased physiological demands such as pregnancy. Inflammation can also lower TSAT by raising hepcidin, which blocks iron absorption and release from stores.
How often should I get my Transferrin Saturation tested?
For individuals without known iron problems, a TSAT check every 1‑2 years is sufficient as part of routine health screening. If you have a history of anemia, chronic disease, or are undergoing treatment for iron deficiency, testing every 3‑6 months until levels normalize, then annually, is advisable.
Can lifestyle changes improve my Transferrin Saturation levels?
Yes. Optimizing diet with iron‑rich foods and vitamin C, spacing calcium and polyphenol intake, and addressing chronic inflammation through weight management, exercise, and stress reduction can all raise TSAT. Adequate sleep and limiting excessive alcohol also support healthy iron metabolism.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.