Understanding Your Neutrophil to Lymphocyte Ratio Results
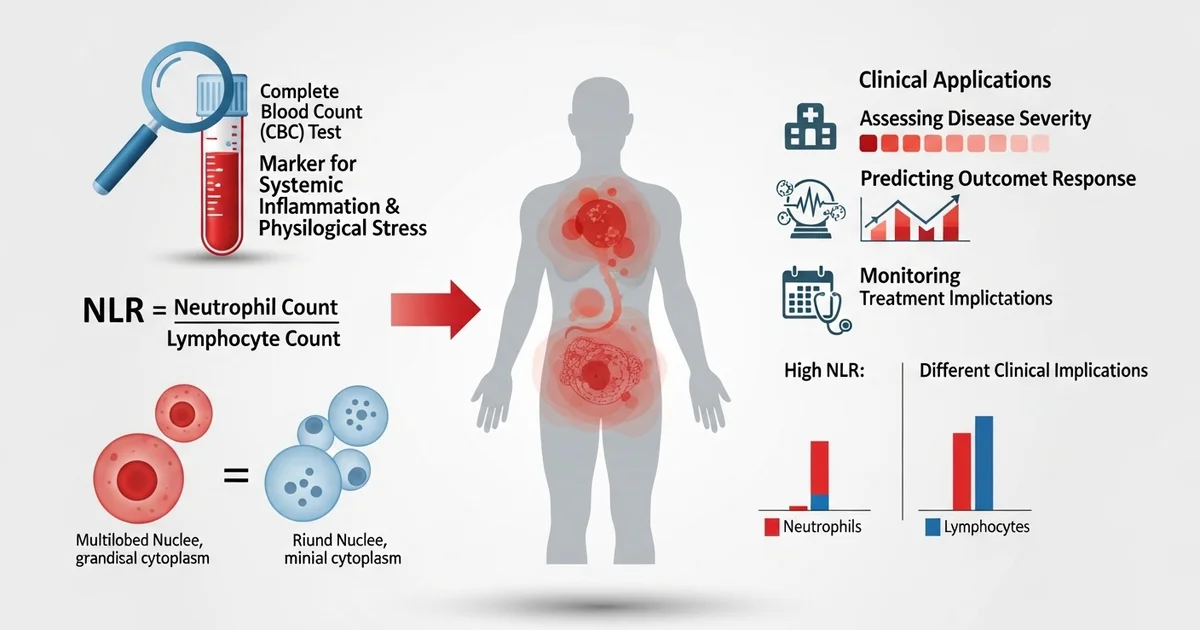
Direct answer: The neutrophil-to-lymphocyte ratio (NLR) is a simple calculation from your complete blood count (CBC) test. It is used as a marker for systemic inflammation and physiological stress in the body. Doctors use the NLR to help assess disease severity, predict outcomes, and monitor treatment response for various conditions, including infections, cardiovascular diseases, and certain cancers. A high NLR often indicates an inflammatory state, while a low ratio is less common and has different clinical implications.
TL;DR The neutrophil-to-lymphocyte ratio (NLR) is a valuable health marker calculated from the neutrophil and lymphocyte counts in your standard blood test. It provides a snapshot of your body's inflammatory status. Neutrophils are your immune system's first responders to infection or injury, while lymphocytes are involved in more specific, long-term immune responses. The balance between them, reflected in the NLR, helps clinicians gauge underlying inflammation and physiological stress, which are linked to many chronic diseases.
- What is the NLR?: It's the number of neutrophils divided by the number of lymphocytes, two types of white blood cells found in a complete blood count (CBC).
- Why it Matters: The NLR is a sensitive, non-specific marker of inflammation. A high ratio suggests a strong inflammatory response, often seen in acute infections, tissue injury, or chronic diseases.
- Normal vs. High Ratio: A typical healthy NLR is between 1 and 3. A ratio consistently above 3 may indicate underlying inflammation or stress that warrants further investigation.
- Clinical Applications: Doctors use the NLR to help assess the severity and prognosis of conditions like heart disease, autoimmune disorders, severe infections (like sepsis), and some cancers.
- Not a Standalone Test: The NLR is not a diagnostic tool on its own. It is always interpreted in the context of your overall health, symptoms, and other lab results.
- Improving Your Ratio: Lifestyle changes that reduce inflammation, such as a balanced diet, regular exercise, stress management, and adequate sleep, can help maintain a healthy NLR.
Want the full explanation? Keep reading ↓
Beyond the Basics: Why Does the Balance Between Neutrophils and Lymphocytes Matter?
The Complete Blood Count (CBC) is one of the most frequently ordered lab tests, providing a wealth of information about your health. While individual cell counts are important, the relationship between different types of white blood cells can offer even deeper insights. The Neutrophil-to-Lymphocyte Ratio (NLR) is a powerful, yet simple, biomarker that does just that.
Neutrophils and lymphocytes are two critical components of your immune system, each with a distinct role. Neutrophils are the "first responders," a key part of the innate immune system that rushes to the site of bacterial infections or tissue injury. In contrast, lymphocytes are the strategists of the adaptive immune system, responsible for orchestrating targeted attacks against specific pathogens like viruses and for creating long-term immune memory.
The NLR provides a snapshot of the balance between these two forces. It serves as an indicator of systemic inflammation and physiological stress, reflecting the body's response to a wide range of conditions, from infections to chronic diseases.
Unlocking the Data: How is the Neutrophil-to-Lymphocyte Ratio Calculated?
The beauty of the NLR lies in its simplicity. It is not a separate, expensive test but is calculated using two values readily available from the differential portion of a standard CBC.
The calculation is straightforward:
NLR = Absolute Neutrophil Count ÷ Absolute Lymphocyte Count
For this calculation, it is crucial to use the absolute counts (often reported as x10³/μL or x10⁹/L) rather than the percentages. Percentages can be misleading because a change in one cell type can alter the percentage of another, even if its absolute number hasn't changed. Using absolute counts provides a more accurate picture of the immune system's status.
What's a Normal NLR? Understanding the Reference Ranges
There is no single, universally accepted "normal" value for the NLR, as the optimal range can be influenced by age, ethnicity, and overall health status. However, extensive research has established generally accepted ranges that help clinicians interpret this value in a clinical context. A lower ratio is generally considered healthier in an asymptomatic individual.
The table below outlines typical NLR reference ranges. It's important to remember that these are guidelines, and your results should always be interpreted by a healthcare provider who understands your complete medical picture.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Healthy Adults | 1.0 - 3.0 | Ratio | Values between 2.0 and 3.0 may be seen as low-grade chronic inflammation. |
| Healthy Older Adults (>65) | 1.2 - 3.5 | Ratio | The ratio tends to increase slightly with age due to "inflammaging." |
| Optimal / Low Risk | < 2.0 | Ratio | Often associated with lower risk for chronic inflammatory conditions. |
| Critically Ill Patients | > 5.0 - 8.0 | Ratio | High values are prognostic indicators; the specific threshold depends on the condition. |
A Red Flag for Inflammation: What Does a High NLR Indicate?
A high NLR is a significant finding that typically points to an underlying state of systemic inflammation or acute physiological stress. It occurs when neutrophil counts rise (neutrophilia) and/or lymphocyte counts fall (lymphopenia). This shift indicates that the body is mounting a strong, immediate inflammatory response while simultaneously suppressing its more targeted, long-term immune functions.
This imbalance is driven by stress hormones like cortisol, which stimulate the bone marrow to release neutrophils while promoting the self-destruction (apoptosis) of lymphocytes. Understanding the different types of lymphocytes—including [T-cells, B-cells, and NK-cells, which are crucial for a coordinated immune response]—helps clarify why their suppression is so significant.
Bacterial Infections and Sepsis
A high NLR is a classic sign of a bacterial infection. The body ramps up neutrophil production to fight invading bacteria, leading to a sharp increase in the ratio.
- Differentiating Infections: The NLR can help distinguish a likely bacterial infection (high NLR) from a viral one, which often presents with a low or normal NLR.
- Prognosis in Sepsis: In sepsis, a life-threatening response to infection, a very high or steadily rising NLR is a poor prognostic sign. It suggests the infection is overwhelming the body's defenses and is associated with a higher risk of organ failure and mortality.
Cardiovascular Disease
Chronic inflammation is a well-established driver of atherosclerosis (the hardening and narrowing of arteries). The NLR serves as a reliable marker of this underlying inflammatory state.
- Predicting Risk: A persistently elevated NLR in otherwise healthy individuals is associated with an increased risk of developing hypertension, coronary artery disease, and stroke.
- Prognostic Value: In patients with known heart disease, a high NLR can predict adverse outcomes, such as heart attack, stent failure, or death. It is often monitored after a cardiac event to gauge the level of systemic stress and inflammation.
Cancer (Oncology)
The NLR has emerged as a powerful prognostic tool in the field of oncology. A high NLR is consistently linked to poorer outcomes across many types of solid tumors, including lung, colorectal, breast, pancreatic, and ovarian cancers.
- Tumor-Related Inflammation: Cancer creates a pro-inflammatory environment that stimulates neutrophil production.
- Suppressed Anti-Tumor Immunity: The corresponding drop in lymphocytes indicates a weakened adaptive immune system, which is less capable of recognizing and destroying cancer cells.
- Monitoring Treatment: Changes in the NLR during chemotherapy or immunotherapy can help predict treatment response. A decreasing NLR may suggest the treatment is working effectively.
Post-Surgical Stress and Trauma
Major surgery, trauma, or severe burns trigger a massive physiological stress response. The body releases a flood of cortisol and other stress hormones.
- Predicting Complications: This hormonal surge drives neutrophil counts up and lymphocyte counts down, resulting in a predictably high NLR.
- Monitoring Recovery: An NLR that remains excessively high or fails to decrease in the days following surgery can be a warning sign for developing complications, such as post-operative infections or poor wound healing.
An Imbalance in the Other Direction: When Is a Low NLR a Concern?
A low NLR is less common and generally less studied than a high NLR, but it can still provide valuable clinical clues. It is caused by either a low neutrophil count (neutropenia) or a high lymphocyte count (lymphocytosis).
Viral Infections
This is one of the most common causes of a temporarily low NLR. Many viruses trigger a robust lymphocyte-driven immune response.
- Lymphocyte Proliferation: The body produces a large number of lymphocytes to identify and clear virus-infected cells, leading to lymphocytosis. To understand why a [high lymphocyte count is common in viral infections], it's helpful to know how these cells target specific pathogens.
- Diagnostic Clue: In a patient with fever and general malaise, a low NLR can strengthen the suspicion of a viral illness over a bacterial one. Conditions like infectious mononucleosis (mono), caused by the Epstein-Barr virus, are classic examples.
Autoimmune Conditions
While some autoimmune disorders are associated with a high NLR due to inflammation, others can present with a low NLR.
- Lupus (SLE): Systemic lupus erythematosus can sometimes cause neutropenia, which would lower the NLR.
- Felty's Syndrome: This rare complication of rheumatoid arthritis is characterized by a triad of rheumatoid arthritis, an enlarged spleen, and a very low neutrophil count.
Medication Side Effects
Certain medications can suppress bone marrow production of neutrophils, leading to drug-induced neutropenia and a low NLR. Common culprits include some types of chemotherapy, certain antibiotics, and anti-thyroid medications.
Underlying Hematological Disorders
In rare cases, a persistently low NLR, particularly due to neutropenia, may signal an issue with the bone marrow's ability to produce cells. This could include conditions like aplastic anemia or certain leukemias and warrants a full hematological workup.
Putting the Pieces Together: How NLR Works with Other Markers
The NLR is a powerful indicator, but it should never be interpreted in isolation. It is most valuable when considered alongside the patient's symptoms, clinical history, and other laboratory tests.
- C-Reactive Protein (CRP): Both NLR and CRP are markers of inflammation. However, the NLR often rises and falls more quickly than CRP, making it a more dynamic marker of acute stress. They provide complementary information about the inflammatory state.
- Total White Blood Cell (WBC) Count: The NLR offers more nuance than the total WBC count. A patient can have a normal total WBC count that masks a dangerous imbalance—for example, high neutrophils and low lymphocytes could cancel each other out, but the resulting high NLR would still signal a problem.
- Platelet-to-Lymphocyte Ratio (PLR): Similar to the NLR, the PLR is another calculated ratio used to assess inflammation and prognosis in various diseases. Sometimes, clinicians look at both markers together for a more comprehensive view.
Context is Key: What Else Can Affect Your NLR?
Before drawing conclusions from an abnormal NLR, it's essential to consider other factors that can influence this ratio. A single reading may not be significant; trends over time are often more informative.
Factors That Can Increase NLR:
- Acute Physiological Stress: Intense exercise, panic attacks, or severe pain.
- Smoking: Chronic smoking induces a state of low-grade inflammation.
- Obesity: Adipose (fat) tissue is metabolically active and releases inflammatory cytokines.
- Poor Sleep / Sleep Apnea: Chronic sleep deprivation is a physiological stressor.
- Certain Medications: Corticosteroids (e.g., prednisone) are well-known to increase neutrophils and decrease lymphocytes.
Factors That Can Decrease NLR:
- Medications: As mentioned, certain drugs can cause neutropenia.
- Nutritional Deficiencies: Severe vitamin B12 or folate deficiency can impair cell production in the bone marrow.
Can I Improve My NLR? Actionable Steps for a Healthier Balance
While you cannot directly control your cell counts, you can influence the underlying factors that contribute to chronic inflammation. If your NLR is elevated due to lifestyle-related inflammation, adopting healthier habits may help bring it into a better range over time.
Focus on an Anti-Inflammatory Lifestyle:
- Diet: Emphasize whole foods rich in antioxidants and omega-3 fatty acids. This includes fruits, vegetables, leafy greens, nuts, seeds, and fatty fish like salmon. Minimize processed foods, sugary drinks, and excessive saturated fats.
- Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity (like brisk walking or cycling) per week, plus strength training. Regular exercise is a potent anti-inflammatory.
- Stress Management: Chronic stress elevates cortisol, which directly increases the NLR. Incorporate stress-reducing practices like mindfulness, meditation, yoga, or deep-breathing exercises into your daily routine.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep per night. Poor sleep is a major driver of inflammation.
- Maintain a Healthy Weight: If you are overweight, losing even a small percentage of your body weight can significantly reduce inflammatory markers.
- Avoid Smoking: Quitting smoking is one of the most impactful things you can do to reduce chronic inflammation.
It's important to discuss any concerns about your NLR with your healthcare provider. They can help determine the cause of an abnormal result and recommend the most appropriate course of action.
Frequently Asked Questions
What is the most common cause of abnormal Lymphocytes levels?
The most common cause of abnormal lymphocyte levels depends on whether they are high or low. High lymphocytes (lymphocytosis) are most frequently caused by acute viral infections, such as the common cold, influenza, or infectious mononucleosis (mono). Low lymphocytes (lymphopenia) are often a temporary result of acute stress, such as a severe bacterial infection, trauma, or surgery, where stress hormones suppress lymphocyte counts. To understand the [normal lymphocyte count and percentage], it's important to compare your results to established reference ranges.
How often should I get my Lymphocytes tested?
For a healthy individual with no symptoms, lymphocyte levels are typically checked as part of a routine Complete Blood Count (CBC) during a physical exam, which may be annually or every few years. If you have a known medical condition that affects the immune system (like an autoimmune disorder or cancer), or if you are undergoing treatment that can impact blood counts (like chemotherapy), your doctor will recommend a much more frequent testing schedule to monitor your condition and response to therapy.
Can lifestyle changes improve my Lymphocytes levels?
Yes, lifestyle can have a significant impact on your immune system's balance, which includes your lymphocyte levels. Chronic stress, poor sleep, and a diet high in processed foods can contribute to chronic inflammation and immune dysregulation, potentially lowering lymphocyte counts over time. Conversely, adopting an anti-inflammatory lifestyle—including a balanced diet rich in fruits and vegetables, regular moderate exercise, effective stress management, and adequate sleep—can support a healthy immune system and help maintain your lymphocyte levels within an optimal range.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.