Understanding Your Monocyte Count and What It Means for You
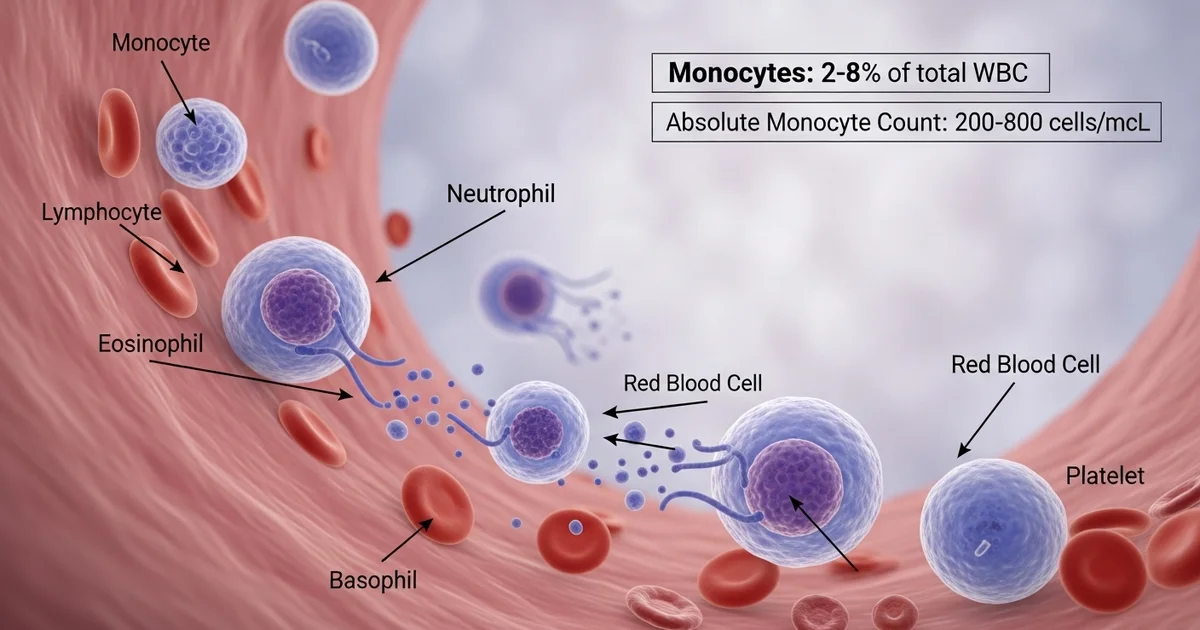
Direct answer: A normal monocyte range is typically 2% to 8% of your total white blood cells. The absolute monocyte count, a more precise measure, normally falls between 200 and 800 cells per microliter of blood (cells/mcL). These values can vary slightly between laboratories. High or low monocyte levels, known as monocytosis or monocytopenia respectively, can indicate infection, inflammation, or other underlying medical conditions that may require further investigation by a healthcare provider.
TL;DR Monocytes are a type of white blood cell crucial for your immune system, acting as cellular 'clean-up crews' that fight off infections and remove dead cells. A complete blood count (CBC) test measures both the percentage of monocytes relative to other white blood cells and the absolute count, which is the total number in a volume of blood. While a normal range is a good indicator of health, deviations can signal an underlying issue that your doctor will want to investigate.
What Are Monocytes?: They are the largest type of white blood cell and play a key role in your immune defense by engulfing pathogens and cellular debris.
Normal Range: A typical monocyte range is 2% to 8% of your white blood cell differential. The absolute count is generally between 200 and 800 cells per microliter (cells/mcL).
High Monocytes (Monocytosis): An elevated count often points to your body fighting a chronic infection, an autoimmune disorder, or certain types of inflammation. It's a sign your immune system is highly active.
Low Monocytes (Monocytopenia): A decreased count is less common but can be caused by conditions that suppress bone marrow function, such as chemotherapy, certain infections, or aplastic anemia.
Why It Matters: Your monocyte count is a valuable piece of your overall health puzzle. It helps doctors identify potential problems, from simple infections to more complex chronic diseases.
Next Steps: Abnormal results are not a diagnosis on their own. Your doctor will interpret them in the context of your full CBC panel, symptoms, and medical history to determine the cause and recommend any necessary follow-up.
Want the full explanation? Keep reading ↓
Normal Monocyte Range and Absolute Count
Monocytes are a crucial type of white blood cell, acting as the versatile "cleanup crew" of your immune system. They are the largest of the white blood cells and play a vital role in fighting off bacteria, viruses, and fungi, as well as removing dead or damaged cells from the body. Understanding your monocyte count, a key component of a Complete Blood Count (CBC), can provide important insights into your health.
While a percentage is often reported, the absolute monocyte count is the most clinically significant measurement. This number reflects the actual quantity of monocytes in a specific volume of blood, offering a more accurate picture of your immune status than a relative percentage, which can fluctuate based on other white blood cell levels. An abnormal count, whether high or low, is not a diagnosis in itself but serves as a critical indicator for your healthcare provider to investigate further.
What is a Normal Monocyte Count?
Defining a "normal" monocyte range is complex, as it can vary based on age, sex, and the specific laboratory conducting the test. It's essential to always compare your results to the reference range provided by the lab that performed your bloodwork.
The absolute monocyte count is measured in cells per microliter of blood (cells/mcL or cells/µL) or as a number per liter (x10⁹/L).
Monocyte Reference Ranges Table
The following table provides typical reference ranges for the absolute monocyte count. Remember, these are general guidelines, and your laboratory's specific range is the most accurate benchmark for your results.
| Population | Normal Range | Units | Notes |
|---|---|---|---|
| Adults | 200 - 800 | cells/mcL | Can be slightly higher in men. |
| Newborns (0-1 month) | 100 - 1,700 | cells/mcL | Ranges are highest at birth and decrease with age. |
| Children (1-18 years) | 100 - 1,000 | cells/mcL | Gradually decreases to adult levels through adolescence. |
| Pregnancy | 200 - 900 | cells/mcL | May increase slightly, especially in the first trimester. |
Worried About a High Monocyte Count? Understanding Monocytosis
When your absolute monocyte count is elevated above the normal reference range, the condition is called monocytosis. This is a common finding and usually indicates that your immune system is actively fighting something. Monocytes are dispatched from the bone marrow to respond to inflammation, infection, or cellular debris.
Monocytosis is rarely a standalone issue. Instead, it’s a signal that points toward an underlying medical condition that requires attention. Your doctor will use this finding, along with your symptoms and other test results, to determine the cause. Learning about the functions of these cells can help you understand why they might be elevated; for a deeper dive, you can explore more about [the monocytes blood test and its role as the body's cleanup crew].
What Causes High Monocytes?
An elevated monocyte count can be triggered by a wide array of conditions, ranging from temporary infections to chronic diseases.
1. Chronic Infections: While acute infections might cause a spike in other white blood cells like neutrophils, monocytes are often elevated in response to long-term or persistent infections.
- Tuberculosis (TB): A classic cause of monocytosis.
- Fungal Infections: Such as histoplasmosis or blastomycosis.
- Bacterial Endocarditis: An infection of the heart valves.
- Syphilis, Brucellosis, and Listeriosis.
2. Autoimmune and Inflammatory Disorders: In these conditions, the immune system mistakenly attacks the body's own tissues, leading to chronic inflammation. Monocytes are key players in this inflammatory process.
- Inflammatory Bowel Disease (IBD): Includes Crohn's disease and ulcerative colitis.
- Rheumatoid Arthritis (RA): Inflammation of the joints.
- Systemic Lupus Erythematosus (SLE): A multi-system autoimmune disease.
- Sarcoidosis: A condition causing inflammatory cell clusters (granulomas) to form in organs, most commonly the lungs.
3. Blood Disorders and Cancers: A persistently high monocyte count can sometimes be a sign of a hematologic (blood-related) disorder.
- Chronic Myelomonocytic Leukemia (CMML): A type of cancer characterized by a very high monocyte count.
- Myelodysplastic Syndromes (MDS): A group of disorders where the bone marrow does not produce enough healthy blood cells.
- Hodgkin's and Non-Hodgkin's Lymphoma.
- Multiple Myeloma.
4. Recovery Phase: An elevated monocyte count can be a positive sign during the recovery phase from certain events.
- Post-Infection: After a significant infection, monocytes help clean up the remaining cellular debris.
- Post-Chemotherapy: As the bone marrow recovers, it may produce a wave of monocytes. This is often called "recovery monocytosis."
5. Other Causes:
- Splenectomy: Removal of the spleen, an organ that filters blood, can lead to a sustained increase in monocytes.
- Certain Medications: Some drugs, including certain growth factors, can stimulate monocyte production.
What are the Symptoms of High Monocytes?
It's important to understand that monocytosis itself does not cause symptoms. The symptoms you might experience are due to the underlying condition that is causing the high monocyte count.
Pay attention to these potential signs and discuss them with your doctor:
- Persistent fatigue or a general feeling of being unwell (malaise).
- Unexplained weight loss.
- Fever or night sweats.
- Swollen lymph nodes in the neck, armpits, or groin.
- Pain or swelling in the joints.
- Abdominal pain or fullness, which could indicate an enlarged spleen.
Concerned About a Low Monocyte Count? Exploring Monocytopenia
A lower-than-normal absolute monocyte count is known as monocytopenia. This condition is less common than monocytosis and often points to an issue with the bone marrow's ability to produce cells. A low count can make you more susceptible to certain types of infections.
Because monocytes are a fundamental part of your immune defense, a significantly low count is a serious finding that warrants a thorough medical evaluation to identify the root cause.
What Causes Low Monocytes?
Monocytopenia is typically linked to conditions that suppress or damage the bone marrow, where all blood cells are made.
- Bone Marrow Suppression or Damage:
- Chemotherapy and Radiation Therapy: These cancer treatments are designed to target rapidly dividing cells, which includes both cancer cells and healthy bone marrow cells.
- Aplastic Anemia: A rare but serious condition where the bone marrow fails to produce enough new blood cells, including monocytes.
- Certain Leukemias:
- Hairy Cell Leukemia: A rare, slow-growing cancer of the blood in which the bone marrow makes too many B-cell lymphocytes, crowding out other cells like monocytes.
- Overwhelming Infections:
- Sepsis: A life-threatening response to infection can sometimes deplete the body's supply of white blood cells, including monocytes, as they are used up faster than they can be produced.
- Medications:
- High-dose corticosteroids (like prednisone): These powerful anti-inflammatory drugs can suppress the immune system and lower monocyte counts.
- Genetic Conditions:
- Rare inherited disorders, such as GATA2 deficiency, can lead to a severe lack of monocytes and increase the risk of infections and certain cancers.
What are the Signs of Low Monocytes?
Similar to monocytosis, monocytopenia does not have its own specific symptoms. The primary concern with a low monocyte count is an increased vulnerability to infection.
The signs are often related to the underlying cause or the resulting weakened immunity:
- Frequent or recurring infections.
- Symptoms of an active infection, such as fever, chills, cough, or sore throat.
- Fatigue, paleness, or easy bruising, which can be signs of a broader bone marrow problem affecting red blood cells and platelets as well.
How Are Monocyte Levels Measured? The Complete Blood Count (CBC)
Your monocyte count is measured as part of a Complete Blood Count (CBC) with differential. This is one of the most common blood tests ordered by doctors. The "differential" part of the test breaks down the different types of white blood cells, including neutrophils, lymphocytes, eosinophils, basophils, and monocytes.
Understanding Absolute vs. Relative Monocyte Count
Your CBC report will likely show two numbers for monocytes:
- Relative Monocyte Count (%): This is the percentage of monocytes in relation to the total number of white blood cells. A typical range is 2% to 8%. This number can be misleading; for example, if your total white blood cell count is very low, your monocyte percentage might appear normal or high even if the actual number of cells is dangerously low.
- Absolute Monocyte Count (AMC): This is the actual number of monocytes in a microliter of blood. This is the most important value for clinical assessment. It provides a direct measurement that isn't influenced by changes in other white blood cell populations.
Always focus on the absolute count when discussing your results with your healthcare provider.
Preparing for Your Monocyte Blood Test
A CBC is a simple blood draw, and generally, no special preparation is needed.
- You typically do not need to fast.
- Stay well-hydrated to make the blood draw easier.
- Inform your doctor of all medications, herbs, and supplements you are taking, as some can affect blood cell counts.
My Monocyte Count is Abnormal. What Happens Next?
An abnormal monocyte count is a starting point, not a conclusion. Your doctor's next steps will be guided by your specific results, your overall health, and any symptoms you may have.
If Your Count is High (Monocytosis)
- Repeat the Test: A single high reading, especially if it's a mild elevation, may be temporary. Your doctor might repeat the CBC in a few weeks to see if the count has returned to normal.
- Review Your History: Your doctor will ask about recent infections, travel history, medications, and any symptoms of chronic inflammatory or autoimmune diseases.
- Further Testing: If the monocytosis is persistent or very high, further tests may be ordered. These can include:
- Inflammatory Markers: C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR) to check for inflammation.
- Peripheral Blood Smear: A pathologist examines a sample of your blood under a microscope to look at the appearance and maturity of your blood cells. This is crucial for identifying abnormal or immature monocytes, which can be a sign of leukemia.
- Specific Infection Testing: Tests for conditions like tuberculosis, EBV (mono), or fungal infections.
- Bone Marrow Biopsy: If a serious blood disorder like leukemia or MDS is suspected, a sample of your bone marrow will be taken for analysis.
If Your Count is Low (Monocytopenia)
- Review Medications: Your doctor will first look at any medications you are taking, especially steroids or chemotherapy agents.
- Assess for Infection: You will be checked for signs of a severe, overwhelming infection.
- Further Testing: Persistent monocytopenia requires a thorough investigation, which may include:
- Peripheral Blood Smear: To look for signs of conditions like hairy cell leukemia.
- Bone Marrow Biopsy: This is a critical test to evaluate the overall health of your bone marrow and diagnose conditions like aplastic anemia or cancer.
- Genetic Testing: If a rare inherited disorder is suspected.
Understanding your monocyte count is an important part of managing your health. By learning about the functions of [monocytes as your body's cleanup crew], you can have more informed discussions with your doctor. Always work with your healthcare provider to interpret your results and create a plan that is right for you.
Frequently Asked Questions
What is the most common cause of abnormal Monocytes levels?
The most common cause of a high monocyte count (monocytosis) is a response to an infection. This can include viral infections like mononucleosis (Epstein-Barr virus), chronic bacterial infections like tuberculosis, or fungal infections. The second most common category of causes includes chronic inflammatory and autoimmune conditions, such as lupus, rheumatoid arthritis, and inflammatory bowel disease. A persistently low count (monocytopenia) is less common and is often linked to treatments that suppress the bone marrow, like chemotherapy, or specific blood disorders.
How often should I get my Monocytes tested?
For a healthy individual with no symptoms, monocyte levels are typically checked only as part of a routine physical examination with a Complete Blood Count (CBC). There is no standard schedule. However, if you have a known medical condition that can affect monocyte levels (like an autoimmune disease or a blood disorder), or if you are undergoing treatment like chemotherapy, your doctor will order tests much more frequently to monitor your condition and response to therapy. If an initial test shows an abnormal result, your doctor will likely schedule a follow-up test within a few weeks or months to see if the level has normalized.
Can lifestyle changes improve my Monocytes levels?
Lifestyle changes are generally not a direct treatment for an abnormal monocyte count, as the count is a reflection of an underlying medical condition. However, a healthy lifestyle can support overall immune function. If your monocytosis is related to chronic inflammation, adopting an anti-inflammatory diet (rich in fruits, vegetables, omega-3 fatty acids) and managing stress may help support your body's efforts to regulate the immune system. If your count is low, the priority is to avoid infection by practicing excellent hygiene, avoiding sick people, and ensuring you are up-to-date on vaccinations as advised by your doctor. Ultimately, the most effective way to normalize your monocyte count is to work with your doctor to diagnose and treat the root cause.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.