Understanding Your Lymphocyte Count and What It Means for You
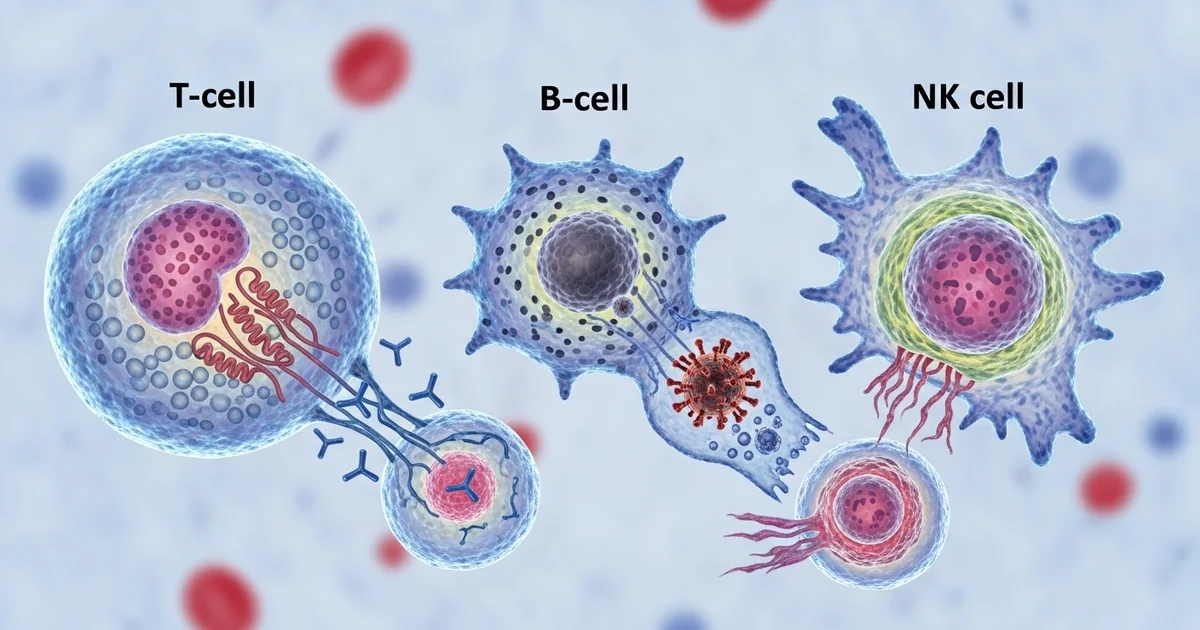
Direct answer: Lymphocytes are a type of white blood cell crucial for your immune system. Found in your blood and lymph tissue, they defend your body against bacteria, viruses, and cancer cells. The main types are T-cells (which attack infected cells), B-cells (which make antibodies), and Natural Killer (NK) cells (which kill tumors and virally infected cells). A complete blood count (CBC) test measures their levels, which can indicate infection, inflammation, or other medical conditions.
TL;DR Lymphocytes are a vital type of white blood cell that forms the core of your adaptive immune system, providing targeted defense against specific threats. They are produced in your bone marrow and circulate through your blood and lymphatic system, ready to identify and destroy pathogens like viruses and bacteria, as well as abnormal cells like cancer. A standard Complete Blood Count (CBC) test measures the number of lymphocytes in your blood, offering a key snapshot of your immune health.
- What are Lymphocytes?: Specialized white blood cells that are essential for immune function, protecting your body from illness.
- Main Types: The three primary types of lymphocytes are T-cells, B-cells, and Natural Killer (NK) cells, each with a unique role in immunity.
- B-Cells: These cells produce antibodies, which are proteins that attach to pathogens, marking them for destruction by other immune cells.
- T-Cells: T-cells directly attack and kill infected cells, help activate other immune cells (Helper T-cells), and regulate the immune response (Regulatory T-cells).
- Natural Killer (NK) Cells: Part of your innate immune system, NK cells provide a rapid response to kill virally infected cells and detect and destroy early signs of cancer.
- Why Levels Matter: Abnormal lymphocyte counts (either too high or too low) can be an important indicator of an underlying health issue, such as an infection, an autoimmune disorder, or certain types of cancer, often prompting further investigation.
Want the full explanation? Keep reading ↓
Feeling Unwell? Your Lymphocyte Count Might Hold the Answer
Lymphocytes are a crucial type of white blood cell that forms the backbone of your adaptive immune system. When you get a Complete Blood Count (CBC) with a differential, the lymphocyte count provides a snapshot of this vital defense force. Understanding what these cells are, what they do, and what their numbers mean is key to interpreting your health status.
These cells are your body’s specialized soldiers, trained to recognize and destroy specific threats like viruses, bacteria, and even cancerous cells. An abnormal count—either too high or too low—is often the first clue that your immune system is fighting an infection, dealing with chronic inflammation, or facing a more serious condition. This article will break down the different types of lymphocytes, explain what high and low levels can mean, and provide actionable information to discuss with your healthcare provider.
What Are Normal Lymphocyte Levels? A Quick Reference
Your lymphocyte count can be reported as an absolute number (the total count in a volume of blood) or as a percentage of your total white blood cells. The absolute lymphocyte count (ALC) is the most clinically important value. Reference ranges can vary slightly between laboratories, but the table below provides typical values.
| Population | Normal Range (Absolute) | Normal Range (Percentage) | Units |
|---|---|---|---|
| Adults | 1,000 - 4,800 | 20 - 40 | cells/µL & % |
| Children (1-4y) | 2,000 - 8,000 | 45 - 75 | cells/µL & % |
| Infants (0-1y) | 3,000 - 9,500 | 50 - 80 | cells/µL & % |
| Older Adults | 800 - 3,800 | 15 - 35 | cells/µL & % |
Note: Children and infants naturally have a higher lymphocyte count than adults. It is crucial to use age-appropriate reference ranges when interpreting results.
Who Are the Soldiers of Your Immune System? Meet the Lymphocytes
Lymphocytes are not a single entity; they are a team of highly specialized cells, each with a distinct role in protecting your body. They originate in the bone marrow and mature in various lymphoid tissues like the thymus, spleen, and lymph nodes. The three main types are T-cells, B-cells, and Natural Killer (NK) cells.
Think of them as different branches of your immune system's military:
| Cell Type | Primary Role | Key Function |
|---|---|---|
| T-Cells | Commanders & Ground Troops | Directly kill infected cells and manage the immune response. |
| B-Cells | Intelligence & Weapons Factory | Produce antibodies to neutralize pathogens. |
| NK Cells | Elite Special Forces | Provide rapid, non-specific killing of infected or cancerous cells. |
T-Cells: The Commanders and Soldiers
T-lymphocytes (T-cells) are the central regulators and effectors of the adaptive immune response. They mature in the thymus gland—hence the "T"—and are trained to distinguish the body's own healthy cells ("self") from foreign invaders or abnormal cells ("non-self").
There are several types of T-cells, each with a specific job:
- Helper T-Cells (CD4+): These are the "commanders" of the immune system. They don't fight invaders directly but activate and direct other immune cells, including B-cells and Cytotoxic T-cells, to mount a coordinated attack. A low CD4+ count is a hallmark of advanced HIV infection.
- Cytotoxic T-Cells (CD8+): These are the "ground troops." Once activated by Helper T-cells, they hunt down and destroy cells that have been infected with viruses or have become cancerous. They are essential for clearing viral infections.
- Regulatory T-Cells (Tregs): These are the "peacekeepers." Their job is to suppress the immune response once a threat has been neutralized, preventing excessive inflammation and autoimmunity (when the immune system attacks the body's own tissues).
B-Cells: The Intelligence and Weapons Factory
B-lymphocytes (B-cells) are responsible for "humoral immunity," the part of the immune system that operates in the body's fluids (or "humors"). They mature in the bone marrow and act as the military's intelligence and weapons manufacturing division.
Their primary functions include:
- Antibody Production: When a B-cell encounters a pathogen, it can transform into a plasma cell. This plasma cell is a highly efficient factory that produces millions of antibodies (also called immunoglobulins).
- Neutralization: Antibodies are Y-shaped proteins that circulate in the blood and other bodily fluids. They bind to specific parts of a pathogen, "tagging" it for destruction by other immune cells or directly neutralizing it by blocking its ability to infect healthy cells.
- Memory Creation: After an infection is cleared, some B-cells become memory B-cells. These long-lived cells "remember" the specific pathogen. If the same invader tries to enter the body again, memory B-cells enable a much faster and stronger antibody response, providing long-term immunity. This is the principle behind vaccination.
Natural Killer (NK) Cells: The Elite Special Forces
Natural Killer (NK) cells are a unique type of lymphocyte that bridges the gap between the innate (non-specific) and adaptive (specific) immune systems. Unlike T-cells and B-cells, they do not need to be "trained" to recognize a specific target. They are your immune system's first responders and elite assassins.
Key features of NK cells:
- Rapid Response: They are always on patrol and can kill threatening cells immediately upon detection, without prior activation. This makes them critical for controlling viral infections and cancer at their earliest stages.
- Innate Recognition: NK cells identify and destroy cells that are missing certain "self" markers on their surface—a common trick used by viruses and cancer cells to evade detection by T-cells.
- Broad Targeting: They are highly effective at eliminating virus-infected cells and tumor cells, playing a crucial role in immune surveillance against cancer.
Why Is My Lymphocyte Count High? Decoding Lymphocytosis
A high lymphocyte count, known as lymphocytosis, means your body has produced an excess of these immune cells. In most cases, this is a normal and healthy response to an infection. Your body is simply ramping up its defenses to fight off an invader.
It's important to distinguish between relative lymphocytosis (a high percentage of lymphocytes but a normal absolute count) and absolute lymphocytosis (a high total number). Absolute lymphocytosis is far more clinically significant. A relative increase can occur when another white blood cell type, like neutrophils, decreases.
Common Causes: Your Body on High Alert
The vast majority of lymphocytosis cases are temporary and caused by the immune system's reaction to a foreign invader.
Viral Infections (Most Common Cause):
- Infectious mononucleosis ("mono"), caused by the Epstein-Barr virus (EBV)
- Cytomegalovirus (CMV)
- Influenza (the flu) and other respiratory viruses
- Hepatitis
- Measles, mumps, and rubella
- Chickenpox (varicella-zoster virus)
Bacterial Infections: While most bacterial infections cause a high neutrophil count, some are known for causing lymphocytosis:
- Pertussis (whooping cough)
- Tuberculosis (TB)
- Brucellosis
Physiological Stress: Intense physical stress can cause a temporary, short-lived spike in lymphocytes. This can be seen after:
- Major surgery
- Trauma or serious injury
- A heart attack
- An epileptic seizure
Serious Causes: When to Be Concerned
While less common, a persistently and significantly high lymphocyte count can signal a more serious underlying condition, particularly a blood cancer. In these cases, the lymphocytes are abnormal (malignant) and are proliferating uncontrollably.
- Chronic Lymphocytic Leukemia (CLL): This is the most common cause of persistent, marked lymphocytosis in older adults. It is a slow-growing cancer where the body produces a large number of mature-looking but dysfunctional B-lymphocytes.
- Acute Lymphoblastic Leukemia (ALL): This is an aggressive cancer more common in children but can occur in adults. It involves the rapid overproduction of immature lymphocytes (lymphoblasts).
- Lymphoma: Some types of lymphoma, which are cancers of the lymph nodes, can "spill" cancerous lymphocytes into the bloodstream, causing lymphocytosis.
- Chronic Inflammatory Conditions: Long-term autoimmune diseases can sometimes lead to a mildly elevated lymphocyte count.
Is a Low Lymphocyte Count Dangerous? Unpacking Lymphocytopenia
A low lymphocyte count, known as lymphocytopenia or lymphopenia, means you have fewer lymphocytes than normal. Since these cells are essential for fighting infection, a significantly low count can leave you vulnerable to a wide range of pathogens, especially viruses.
Mild and temporary drops in lymphocytes are common during acute illnesses like the flu or COVID-19. However, a chronic or severe deficiency requires careful medical evaluation to determine the cause and manage the associated risks.
Acquired Causes: What Can Deplete Your Lymphocytes?
Most cases of lymphocytopenia are acquired, meaning they develop at some point in life due to an illness, treatment, or other external factor.
Viral Infections: While many viruses cause lymphocytosis, some can lead to lymphocytopenia.
- HIV (Human Immunodeficiency Virus): This virus specifically targets and destroys CD4+ Helper T-cells, leading to a progressive decline in lymphocyte function and count.
- Influenza and COVID-19: During the acute phase of these illnesses, lymphocytes can be temporarily depleted.
- Hepatitis and Sepsis: Severe systemic infections can overwhelm the immune system and consume lymphocytes.
Medications: Certain drugs are well-known for suppressing the immune system and lowering lymphocyte counts.
- Corticosteroids (e.g., prednisone): Widely used for inflammation, these powerful drugs can cause a rapid drop in lymphocytes.
- Chemotherapy and Radiation Therapy: These cancer treatments target rapidly dividing cells, which includes both cancer cells and healthy lymphocytes.
- Immunosuppressants: Drugs used to prevent organ transplant rejection or treat autoimmune diseases are designed to dampen the immune response, often by reducing lymphocyte numbers.
Autoimmune Disorders: In these conditions, the immune system mistakenly attacks the body's own tissues, which can include lymphocytes.
- Lupus (Systemic Lupus Erythematosus)
- Rheumatoid Arthritis
- Myasthenia Gravis
Nutritional Deficiencies: Severe malnutrition can impair the body's ability to produce immune cells.
- Zinc Deficiency: Zinc is critical for T-cell development and function.
- Protein-Calorie Malnutrition: A lack of basic building blocks prevents the production of all cell types, including lymphocytes.
Inherited Causes: Are You Born With It?
In rare cases, lymphocytopenia is caused by a genetic disorder that affects the development or function of the immune system. These conditions are typically diagnosed in infancy or early childhood due to recurrent, severe infections.
- Severe Combined Immunodeficiency (SCID): Often called "bubble boy disease," this is a group of rare genetic disorders characterized by a profound lack of functional T-cells and B-cells.
- DiGeorge Syndrome: A chromosomal disorder that can result in poor development of the thymus gland, leading to a low T-cell count.
- Wiskott-Aldrich Syndrome: A genetic immunodeficiency that affects both lymphocytes and platelets.
What Should I Do About My Lymphocyte Results?
An abnormal lymphocyte count is a laboratory finding, not a diagnosis. It is a signal that requires further investigation by a healthcare professional.
Checklist for Your Doctor's Visit:
- Bring the Lab Report: Have the full CBC with differential report available. Your doctor will look at the absolute lymphocyte count, not just the percentage.
- Review Other Blood Counts: Your doctor will evaluate your lymphocyte count in the context of your other white blood cells (neutrophils, eosinophils), red blood cells, and platelets.
- Discuss Your Symptoms: Be prepared to talk about any recent or ongoing symptoms, such as fever, fatigue, swollen lymph nodes, night sweats, or unexplained weight loss.
- List Your Medications: Provide a complete list of all prescription drugs, over-the-counter medications, and supplements you are taking.
- Share Your Medical History: Mention any past infections, autoimmune conditions, or family history of blood disorders.
Based on this information, your provider may recommend:
- Watchful Waiting: If the abnormality is mild and you have a clear reason (like a recent viral infection), your doctor may simply repeat the test in a few weeks to see if it has normalized.
- Further Blood Tests: This may include tests for specific viruses (like EBV or CMV), inflammatory markers, or a more detailed analysis of lymphocyte subsets (e.g., CD4/CD8 count).
- Peripheral Blood Smear: A pathologist will manually examine your blood under a microscope to look for abnormal-looking lymphocytes, which can help diagnose leukemia.
- Referral to a Specialist: If a serious condition is suspected, you may be referred to a hematologist (blood disorder specialist) or an immunologist.
Frequently Asked Questions
What is the most common cause of abnormal Lymphocytes levels?
For a high lymphocyte count (lymphocytosis), the most common cause by far is a viral infection. When your body detects a virus like the one that causes infectious mononucleosis (mono), the flu, or a common cold, it ramps up the production of lymphocytes to fight it off. This is a normal, healthy immune response, and the count typically returns to normal after the infection resolves.
For a low lymphocyte count (lymphocytopenia), a common cause is also an acute viral infection, such as influenza or COVID-19, which can temporarily deplete lymphocyte levels. However, persistent or severe lymphocytopenia is often linked to other factors, such as medications (especially corticosteroids and chemotherapy), chronic infections like HIV, or autoimmune disorders like lupus.
How often should I get my Lymphocytes tested?
There is no standard recommendation for the general population to get their lymphocytes tested at a specific interval. A lymphocyte count is typically checked as part of a Complete Blood Count (CBC) with differential, which is ordered by a healthcare provider for specific reasons.
You may have your lymphocytes tested:
- As part of a routine health check-up.
- To investigate symptoms like fatigue, fever, bruising, or recurrent infections.
- To monitor a known medical condition, such as an autoimmune disease, a blood disorder like CLL, or an infection like HIV.
- To monitor the effects of a treatment, such as chemotherapy or immunosuppressive therapy.
Your doctor will determine if and when you need this test based on your individual health status, symptoms, and medical history.
Can lifestyle changes improve my Lymphocytes levels?
Yes, certain lifestyle changes can support a healthy immune system and potentially help maintain normal lymphocyte levels, although they cannot correct a serious underlying medical condition causing an abnormal count. If you have a mild abnormality or want to support overall immune health, consider the following:
- Balanced Nutrition: Ensure adequate intake of protein, vitamins, and minerals. Zinc and protein are particularly crucial for lymphocyte production and function. A diet rich in fruits, vegetables, lean proteins, and whole grains is beneficial.
- Adequate Sleep: Chronic sleep deprivation can suppress immune function and negatively impact lymphocyte activity. Aim for 7-9 hours of quality sleep per night.
- Stress Management: Chronic stress releases cortisol, a hormone that can suppress and destroy lymphocytes. Practices like mindfulness, meditation, yoga, and regular exercise can help manage stress levels.
- Moderate Exercise: Regular, moderate physical activity can enhance immune circulation and function. However, overly strenuous exercise without adequate recovery can temporarily suppress the immune system.
- Avoid Smoking and Excessive Alcohol: Both smoking and excessive alcohol consumption are toxic to immune cells and can impair their ability to function correctly.
It is critical to understand that while these lifestyle measures support general health, they are not a substitute for medical treatment for conditions like leukemia, HIV, or severe immunodeficiencies. Always follow your healthcare provider's advice for managing abnormal lymphocyte counts.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.