Understanding Your Monocyte Count and Its Role in Your Health
Direct answer: Monocytes are a type of white blood cell, crucial for your immune system. They fight off infections, remove dead cells, and help heal tissues. When monocyte levels are too high or too low, it can signal an underlying health issue, including infections, inflammatory conditions, or even autoimmune diseases. A complete blood count (CBC) test measures your monocyte levels, providing important clues about your immune health and potential disorders that may require further investigation by your doctor.
TL;DR Monocytes are a vital part of your immune system, acting as the body's 'clean-up crew' and first responders to threats. These large white blood cells circulate in your bloodstream before moving into tissues, where they transform into macrophages or dendritic cells. Their primary job is to engulf and destroy pathogens like bacteria and viruses, clear away dead cells, and signal other immune cells to join the fight. While essential for protection, their dysregulation is linked to chronic inflammation and autoimmune disorders.
- Monocytes are produced in the bone marrow and make up 2-8% of your white blood cells.
- They are key players in phagocytosis, the process of consuming harmful invaders and cellular debris.
- Once in tissues, they become macrophages, which are powerful defenders against infection and inflammation.
- High monocyte counts (monocytosis) can indicate chronic infections, inflammatory conditions, or certain cancers.
- Low monocyte counts (monocytopenia) are less common but can result from bone marrow issues or certain medical treatments.
- In autoimmune diseases like rheumatoid arthritis or lupus, overactive monocytes can mistakenly attack the body's own healthy tissues.
- A simple Complete Blood Count (CBC) test measures your monocyte levels, offering a window into your immune function.
Want the full explanation? Keep reading ↓
Role of Monocytes in Immunity and Autoimmune Disease
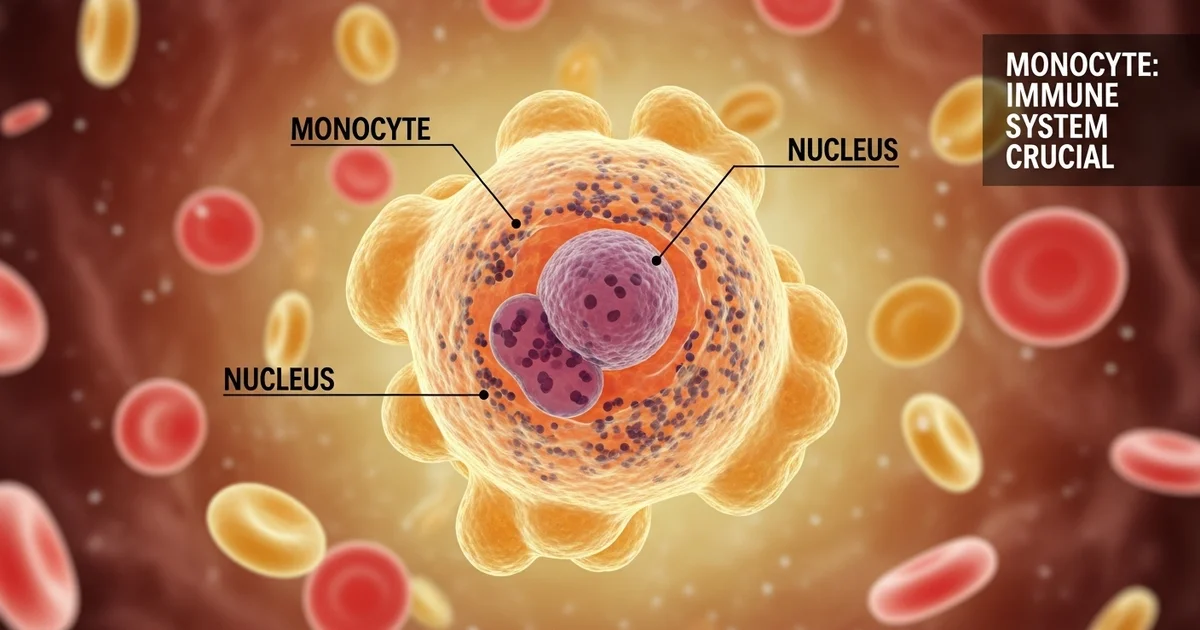
Monocytes are a type of white blood cell, or leukocyte, that play a central and complex role in the body's defense system. As the largest of all white blood cells, they are far more than just passive responders; they are versatile, intelligent cells that act as sentinels, cleanup crews, and commanders in the intricate battle for your health.
While essential for fighting off infections and healing tissues, this same power can be turned against the body, making monocytes key players in the development and progression of autoimmune diseases. Understanding this dual role is crucial for interpreting blood test results and managing chronic inflammatory conditions.
Understanding Your Monocyte Count: What Do the Numbers Mean?
Your monocyte level is typically measured during a complete blood count (CBC) with a differential test. This common blood panel provides a detailed breakdown of your different white blood cells. A [monocytes blood test reveals a lot about the body's cleanup crew] and its inflammatory status.
Results are usually reported in two ways: a relative percentage (%) and an absolute count. While the percentage shows the proportion of monocytes relative to other white blood cells, the absolute monocyte count is the most clinically important value. It provides the actual number of monocytes in a specific volume of blood, offering a more accurate picture of their status.
Monocyte Reference Ranges
Reference ranges can vary slightly between laboratories depending on the equipment and population they serve. The following table provides typical values for adults, but you should always compare your results to the specific range provided by your lab. To understand these values in greater detail, it's helpful to learn about the [normal monocyte range and absolute count] specifically.
| Population | Relative Range (% of WBCs) | Absolute Range (cells/mcL) | Notes |
|---|---|---|---|
| Adult | 2% - 8% | 200 - 800 | The absolute count is more clinically significant. |
| Newborn | 5% - 13% | 400 - 3100 | Levels are naturally higher at birth and decrease with age. |
| Child (1-4 years) | 2% - 7% | 200 - 700 | Values stabilize to adult levels during childhood. |
| Pregnancy | Varies | Can be slightly elevated | Mild increases can occur, especially in the first trimester. |
WBCs = White Blood Cells; mcL = microliter
Monocytes on the Front Lines: How Do They Defend the Body?
Monocytes are produced in the bone marrow and released into the bloodstream. They circulate for only a few days before they migrate into various tissues throughout the body. Once they leave the blood, they undergo a remarkable transformation, differentiating into two main types of highly specialized cells: macrophages and dendritic cells.
This process allows them to perform several critical functions for the innate and adaptive immune systems.
From Monocyte to Macrophage: The Tissue Transformer
When a monocyte settles into a tissue, it often becomes a macrophage. The term "macrophage" literally means "big eater," which perfectly describes its primary function: phagocytosis.
Key Roles of Macrophages:
- Engulfing Pathogens: They are experts at identifying and swallowing bacteria, viruses, fungi, and parasites.
- Clearing Cellular Debris: Macrophages clean up dead or dying cells (a process called apoptosis), preventing the buildup of waste that could trigger inflammation.
- Wound Healing: They play a vital role in tissue repair by clearing away damaged tissue and releasing growth factors that promote healing.
- Iron Recycling: Specialized macrophages in the spleen and liver break down old red blood cells and recycle their iron for use in new cells.
The Sentinel Role: Monocytes as Antigen-Presenting Cells (APCs)
Beyond just "eating" invaders, monocytes and their derivatives act as critical messengers. After engulfing a pathogen, they process it and display fragments of it (called antigens) on their surface. They then travel to lymph nodes to "present" these antigens to T-lymphocytes, the masterminds of the adaptive immune system.
This antigen presentation is the crucial bridge between the immediate, non-specific innate immune response and the highly specific, long-lasting adaptive immune response.
The process works like this:
- Surveillance: A monocyte or macrophage identifies and engulfs an invader (e.g., a bacterium).
- Processing: Inside the cell, the bacterium is broken down into small pieces (antigens).
- Display: The macrophage displays these antigens on its surface using special molecules called MHC-II.
- Activation: The macrophage presents the antigen to a helper T-cell, activating it.
- Coordination: The activated T-cell then orchestrates a targeted attack, involving B-cells (to make antibodies) and cytotoxic T-cells (to kill infected cells).
When Levels Are High: Is Monocytosis a Sign of Trouble?
An elevated monocyte count, known as monocytosis, is not a disease in itself but rather a signal from the body that it is fighting something off. It indicates that the bone marrow is producing more monocytes to meet a demand somewhere in the body. Understanding what a diagnosis of [high monocytes, or monocytosis, means for chronic infection and inflammation] is key to addressing the root cause.
A persistently high monocyte count warrants a thorough medical evaluation to identify the underlying issue.
Common Causes of High Monocytes: From Infection to Inflammation
Monocytosis is most often a response to chronic conditions rather than acute, short-term illnesses.
Primary Causes of Monocytosis:
- Chronic Infections: The body ramps up monocyte production to fight persistent invaders.
- Tuberculosis
- Fungal infections (e.g., Aspergillosis, Histoplasmosis)
- Bacterial endocarditis (infection of the heart valves)
- Syphilis
- Autoimmune and Inflammatory Diseases: Conditions where the immune system is chronically activated.
- Systemic Lupus Erythematosus (SLE)
- Rheumatoid Arthritis (RA)
- Inflammatory Bowel Disease (IBD), including Crohn's disease and ulcerative colitis
- Sarcoidosis
- Blood and Bone Marrow Disorders: Certain cancers originate from or involve monocytes.
- Chronic Myelomonocytic Leukemia (CMML) is characterized by a persistently high monocyte count.
- Hodgkin's and non-Hodgkin's lymphoma
- Myelodysplastic syndromes (MDS)
- Recovery Phase: Monocyte counts can temporarily spike as the body cleans up debris after a severe infection, surgery, or chemotherapy.
What Should You Do About High Monocytes?
If your blood test shows monocytosis, it is essential not to panic. A single elevated reading may be temporary. Your healthcare provider will interpret the result in the context of your overall health, symptoms, and other lab values.
Next Steps May Include:
- Repeating the CBC: To see if the elevation is persistent.
- Reviewing Your Health History: Discussing any recent infections, new symptoms, or chronic conditions.
- Further Testing: This may include inflammatory markers (like CRP and ESR), specific tests for infections, or imaging studies.
- Referral to a Specialist: Depending on the suspected cause, you may be referred to a hematologist (blood disorder specialist) or a rheumatologist (autoimmune specialist).
The Dark Side of Monocytes: Their Role in Autoimmune Disease
In a healthy immune system, monocytes and macrophages can distinguish between "self" (the body's own cells) and "non-self" (invaders). In autoimmune diseases, this system of self-tolerance breaks down. Monocytes, with their powerful inflammatory and tissue-remodeling capabilities, become central figures in the ensuing damage.
They transform from protectors into aggressors, contributing directly to the chronic inflammation and tissue destruction characteristic of these conditions.
How Do Monocytes Drive Autoimmune Attacks?
The malfunction of monocytes in autoimmunity is a multi-step process. Instead of resolving inflammation, they perpetuate it.
- Dysfunctional Debris Clearance: One of the earliest steps in many autoimmune diseases is a failure of macrophages to properly clear away dead and dying cells. This leaves an accumulation of cellular debris and "self-antigens" that the immune system can mistakenly identify as a threat.
- Mistaken Identity and Antigen Presentation: Monocytes and macrophages engulf this self-debris and, in a critical error, present these self-antigens to T-cells. This is like a security guard mistakenly identifying the homeowner as an intruder and calling for an attack.
- Pro-Inflammatory Cytokine Release: Once activated, these monocytes and macrophages release a flood of powerful inflammatory signaling molecules called cytokines (such as TNF-alpha, IL-1, and IL-6). These cytokines recruit more immune cells to the site, creating a vicious cycle of inflammation and tissue damage.
Monocytes in Specific Autoimmune Conditions: A Closer Look
The specific role of monocytes can vary depending on the disease and the tissues affected.
- Rheumatoid Arthritis (RA): Monocytes are heavily recruited to the synovial fluid of joints. There, they differentiate into inflammatory macrophages that release enzymes and cytokines, directly contributing to the erosion of cartilage and bone.
- Systemic Lupus Erythematosus (SLE): In lupus, the failure to clear apoptotic cells is a key trigger. Monocytes are implicated in the development of skin rashes and severe kidney damage (lupus nephritis), where they infiltrate the kidneys and drive inflammation.
- Multiple Sclerosis (MS): Monocytes cross the blood-brain barrier and enter the central nervous system. They become aggressive macrophages that strip the myelin sheath from nerve fibers, leading to the neurological symptoms of MS.
- Inflammatory Bowel Disease (IBD): An abnormal monocyte response to gut bacteria is thought to be a major driver of the chronic intestinal inflammation seen in Crohn's disease and ulcerative colitis.
Can Monocyte Function Be Targeted for Treatment?
Because monocytes are so central to autoimmune inflammation, they have become a major target for modern therapies. Many of the most effective biologic drugs used to treat conditions like RA, IBD, and psoriasis work by blocking the activity of monocytes or the cytokines they produce.
Examples of Monocyte-Targeted Therapies:
- TNF-alpha Inhibitors: These drugs block TNF-alpha, a key inflammatory cytokine produced by macrophages.
- IL-1 and IL-6 Inhibitors: These medications block other critical cytokines released by activated monocytes.
- Cell-Depleting Therapies: Some treatments work by reducing the number of monocytes or preventing them from migrating into tissues.
Research continues to explore more precise ways to "re-educate" dysfunctional monocytes, aiming to restore their protective functions while dampening their destructive capabilities. Modulating their behavior, rather than simply blocking them, represents the future of autoimmune therapy.
Frequently Asked Questions
What is the most common cause of abnormal Monocytes levels?
The most common cause of high monocytes (monocytosis) is a chronic inflammatory or infectious condition. This includes persistent viral or bacterial infections (like tuberculosis or endocarditis), autoimmune diseases (like lupus or rheumatoid arthritis), and certain types of blood cancers. A temporary spike can also occur as the body recovers from an acute infection. Low monocytes (monocytopenia) is much less common and is often associated with bone marrow issues, such as aplastic anemia, or certain hairy-cell leukemia treatments.
How often should I get my Monocytes tested?
For a healthy individual with no symptoms, monocyte levels are checked as part of a routine complete blood count (CBC) during an annual physical or as deemed necessary by a doctor. If you have been diagnosed with a chronic inflammatory condition, autoimmune disease, or blood disorder, your doctor will establish a regular testing schedule to monitor disease activity and your response to treatment. This could range from every few weeks to every few months.
Can lifestyle changes improve my Monocytes levels?
Yes, to an extent. Because monocyte levels often reflect underlying inflammation, lifestyle changes that reduce chronic inflammation can help normalize them. This includes adopting an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids; engaging in regular, moderate exercise; managing stress through techniques like mindfulness or yoga; and getting adequate sleep. However, lifestyle changes cannot replace medical treatment for the underlying cause of abnormal monocyte levels, such as a serious infection or autoimmune disease.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.