Understanding Your RDW Blood Test and What It Means for Your Heart
Direct answer: Yes, emerging research suggests that a high Red Cell Distribution Width (RDW) can be an independent predictor of adverse outcomes in patients with heart disease, including heart failure and coronary artery disease. While not a standalone diagnostic tool, an elevated RDW value on a complete blood count (CBC) test may signal underlying inflammation or oxidative stress, which are linked to cardiovascular risks. It helps doctors assess a patient's overall prognosis and potential for future cardiac events.
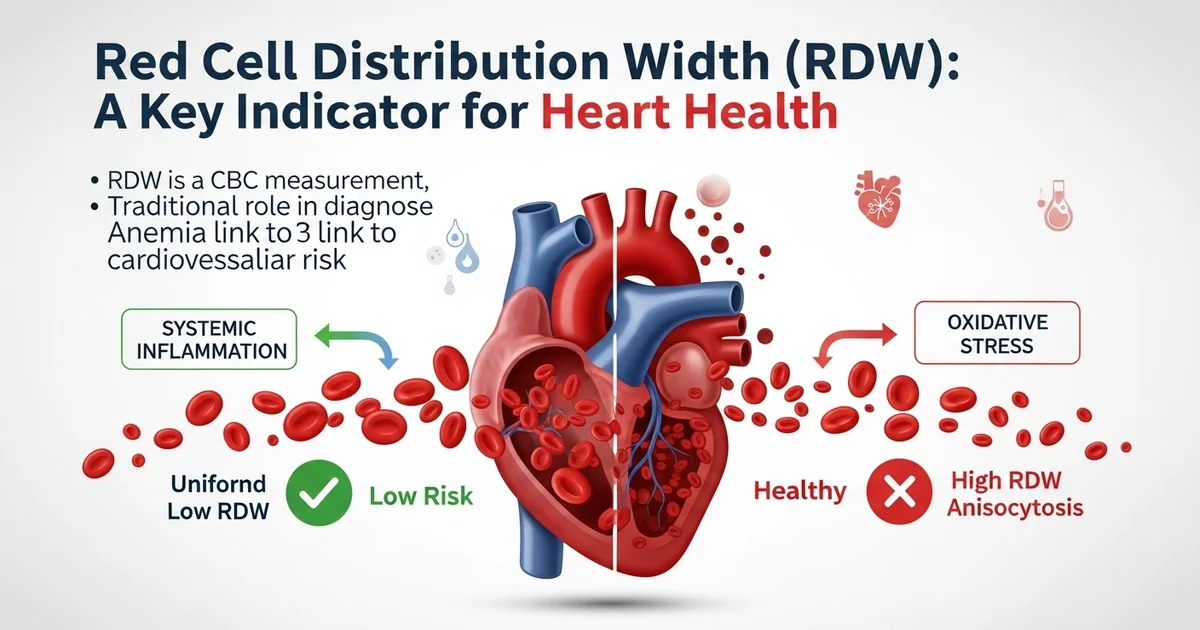
TL;DR Red Cell Distribution Width (RDW) is a standard measurement in a complete blood count (CBC) that indicates the variation in the size of your red blood cells. While traditionally used to help diagnose different types of anemia, recent studies have revealed a significant link between a high RDW and an increased risk for heart disease. A higher RDW suggests greater inconsistency in red blood cell size, a condition called anisocytosis, which can be a sign of underlying systemic inflammation or stress that contributes to cardiovascular problems.
- RDW measures the size variation in your red blood cells, not the cells' actual size.
- A high RDW value is increasingly recognized as an independent risk marker for cardiovascular events, including heart attack and stroke.
- It is not a diagnostic tool for heart disease on its own but adds valuable prognostic information to a patient's overall risk profile.
- The connection is thought to be related to chronic inflammation and oxidative stress, which can affect both red blood cell production and cardiovascular health.
- An elevated RDW has been linked to worse outcomes in patients with existing conditions like heart failure, atrial fibrillation, and coronary artery disease.
- Doctors may use your RDW level, alongside other markers like C-reactive protein (CRP), to get a more complete picture of your cardiovascular risk.
Want the full explanation? Keep reading ↓
Can RDW Predict Heart Disease Risks?
A routine blood test, often overlooked, is gaining significant attention in the world of cardiology. The Red Cell Distribution Width (RDW), a standard component of the Complete Blood Count (CBC), is emerging as a powerful and independent predictor of cardiovascular health. While traditionally used to help diagnose different types of anemia, researchers have discovered that a high RDW may be an early warning sign for a range of heart-related conditions.
This article explores the compelling evidence linking RDW to heart disease, what a high RDW value means for your health, and the practical steps you can take to address this important biomarker. Understanding this connection can empower you to have more informed discussions with your healthcare provider about your cardiovascular risk profile.
What Does an RDW Blood Test Actually Measure?
Before diving into its connection with heart disease, it's crucial to understand what RDW represents. The RDW measures the variation in the size of your red blood cells. In a healthy state, your red blood cells should be relatively uniform in size. However, certain medical conditions can cause significant size variation, a state known as anisocytosis.
The [RDW blood test is a key part of evaluating red blood cell health] because it quantifies this variation. A low RDW means your red blood cells are mostly the same size, which is normal. A high RDW indicates a greater degree of variation, suggesting that something may be disrupting the normal production or survival of these essential cells.
Understanding Your RDW Results: The Normal Ranges
Your lab report will show your RDW value, which is typically reported as a percentage (RDW-CV) or in femtoliters (RDW-SD). While RDW-CV (Coefficient of Variation) is more common, both serve to quantify red blood cell size variability. It is essential to compare your result to the specific reference range provided by the laboratory that performed the test.
However, general reference ranges can provide a helpful baseline for understanding your results. For a deeper dive into these measurements, you can learn more about the [normal RDW range and the SD vs. CV distinction explained] in detail.
RDW Reference Range Table
| Parameter | Normal Range | Units | Notes |
|---|---|---|---|
| RDW-CV | 11.5 - 15.4 | % | Coefficient of Variation. This is the most commonly reported value. |
| RDW-SD | 39 - 46 | fL | Standard Deviation. A direct measurement of size variation. |
| Note | Ranges can vary | Always refer to your specific lab report's reference range. |
A value above the upper limit of the normal range is considered a "high RDW" and warrants further investigation, especially when viewed in the context of your overall health and other lab results.
High RDW Levels? The Link to Heart Disease Explained
A growing body of scientific evidence has established a significant link between an elevated RDW and an increased risk of poor outcomes in patients with cardiovascular disease. Importantly, studies have shown that RDW is an independent predictor of mortality. This means that even after accounting for other known risk factors like age, cholesterol levels, and blood pressure, a high RDW still provides valuable prognostic information.
For individuals with established heart conditions, a high RDW often signals a more severe disease state and a higher likelihood of future adverse events. For the general population, it may serve as an early, subtle indicator of underlying systemic stress that could eventually manifest as heart disease.
What Cardiovascular Conditions Are Linked to High RDW?
Elevated RDW has been associated with a higher risk of incidence, severity, and mortality across a spectrum of cardiovascular diseases.
- Heart Failure (HF): This is one of the strongest associations. Patients with heart failure and a high RDW have a significantly higher risk of hospitalization and mortality compared to those with normal RDW. It reflects a more advanced and unstable disease state.
- Coronary Artery Disease (CAD): In individuals with stable CAD or those experiencing an acute coronary syndrome (like a heart attack), a high RDW is linked to more complex blockages and a greater risk of major adverse cardiac events (MACE), including death or a future heart attack.
- Atrial Fibrillation (AFib): Research indicates that a high RDW is associated with an increased risk of developing AFib. In patients who already have AFib, it is linked to a higher risk of stroke.
- Peripheral Artery Disease (PAD): Similar to CAD, an elevated RDW in patients with PAD—a condition of narrowed arteries in the limbs—is a predictor of worse outcomes and higher mortality.
- Hypertension: Some studies suggest a correlation between high RDW and the development and severity of high blood pressure, possibly due to the role of arterial stiffness and inflammation.
Why Is High RDW a Warning Sign for Your Heart?
The exact mechanisms connecting high RDW to poor cardiovascular outcomes are complex and multifaceted, but researchers have identified several key biological pathways. A high RDW is not the cause of heart disease itself; rather, it is a reflection of underlying pathological processes that are detrimental to the heart and blood vessels.
The Role of Inflammation and Oxidative Stress
Chronic, low-grade inflammation and oxidative stress are foundational pillars of atherosclerosis (the buildup of plaque in arteries) and heart failure.
- Systemic Inflammation: Inflammatory cytokines (signaling molecules) can directly suppress the bone marrow's ability to produce healthy red blood cells. This disruption, known as ineffective erythropoiesis, leads to the premature release of red blood cells of varying sizes, thus increasing RDW.
- Oxidative Stress: This is an imbalance between damaging free radicals and the body's ability to neutralize them with antioxidants. Oxidative stress damages red blood cell membranes, making them more fragile and reducing their lifespan. The body's attempt to compensate by rapidly producing new cells results in greater size variability and a higher RDW.
Nutrient Deficiencies as a Common Culprit
The classic interpretation of a high RDW is rooted in hematology, specifically the diagnosis of anemia. These same deficiencies can also contribute to cardiovascular risk.
- Iron, Vitamin B12, and Folate: These micronutrients are absolutely essential for the synthesis of DNA and the proper maturation of red blood cells.
- Impact on RDW: A deficiency in any of these nutrients leads to impaired red blood cell production. For instance, iron deficiency causes the production of small red blood cells (microcytosis), while B12/folate deficiency leads to large ones (macrocytosis). When these abnormal cells mix with normal cells, the overall size variation—and therefore the RDW—increases.
- Early Detection: A [high RDW can be an early sign of anemia or nutrient deficiency], often appearing before other markers like hemoglobin drop. Addressing these deficiencies is critical for both blood health and cardiovascular wellness.
Poor Red Blood Cell Deformability
A high RDW can also be a marker of reduced red blood cell "deformability" or flexibility. Healthy red blood cells are incredibly flexible, able to squeeze through the body's tiniest capillaries to deliver oxygen.
- Stiff, Fragile Cells: The same inflammatory and oxidative stress that raises RDW also makes red blood cells stiffer and more brittle.
- Microvascular Impairment: These less-flexible cells can struggle to navigate the microcirculation of the heart muscle. This can lead to blockages, reduced oxygen delivery (hypoxia), and further damage to cardiac tissue, worsening conditions like heart failure and contributing to damage during a heart attack.
Worried About Your RDW and Heart Health? Here Are Your Next Steps
Seeing a high RDW on your lab report can be concerning, but it's important to approach it systematically. The key is to view it not as a diagnosis, but as a prompt for a deeper conversation with your doctor.
Step 1: Discuss Your Full CBC Results with Your Doctor
RDW should never be interpreted in isolation. Its meaning is unlocked when viewed alongside other components of the Complete Blood Count, particularly the Mean Corpuscular Volume (MCV), hemoglobin, and hematocrit.
Checklist: Questions to Ask Your Doctor
- What is my specific RDW value, and is it high for this lab's range?
- How does my RDW relate to my MCV? (e.g., a high RDW with a low MCV often points to iron deficiency).
- Are my hemoglobin and hematocrit levels normal?
- Considering my personal health, family history, and other risk factors, what are the most likely causes of this elevated RDW?
- What follow-up tests do you recommend?
Step 2: Investigate the Underlying Cause
The goal is not to "lower the RDW number" but to identify and manage the root cause. Based on your initial results and clinical picture, your doctor may order additional tests to investigate further.
Potential Follow-up Tests:
- Iron Panel: Includes Ferritin, Serum Iron, and Total Iron-Binding Capacity (TIBC) to check for iron deficiency.
- Vitamin Levels: Tests for Vitamin B12 and Folate to rule out deficiencies.
- Inflammatory Markers: C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR) can help quantify systemic inflammation.
- Kidney and Liver Function: Panels to ensure these organs, which are vital for blood health, are functioning properly.
- Cardiovascular Evaluation: Depending on your risk profile, your doctor may suggest an EKG, stress test, or other cardiac imaging.
Step 3: Focus on Heart-Healthy Lifestyle Changes
Regardless of the specific cause, a high RDW often reflects a state of systemic stress. Adopting a heart-healthy lifestyle can help mitigate the underlying inflammation and nutrient issues that contribute to both a high RDW and cardiovascular disease.
Actionable Lifestyle Strategies:
- Eat a Nutrient-Dense Diet: Focus on whole foods rich in iron, B vitamins, and antioxidants. This includes leafy greens, lean meats, fish, legumes, fruits, and vegetables.
- Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity exercise per week, as recommended by the American Heart Association. Exercise helps reduce inflammation and improve cardiovascular function.
- Manage Chronic Conditions: Work closely with your doctor to effectively manage conditions like diabetes, hypertension, and kidney disease, as these can all contribute to a high RDW.
- Avoid Smoking and Limit Alcohol: Both smoking and excessive alcohol consumption promote oxidative stress and inflammation, directly impacting red blood cell health and cardiovascular risk.
- Prioritize Stress Management and Sleep: Chronic stress and poor sleep can exacerbate inflammation. Techniques like mindfulness, yoga, and ensuring 7-9 hours of quality sleep per night are beneficial.
Frequently Asked Questions
What is the most common cause of abnormal Red Cell Distribution Width (RDW) levels?
The most common and classic cause of a high RDW is iron deficiency anemia. Iron is a critical component for producing healthy, uniform red blood cells. When iron stores are low, the bone marrow produces smaller, paler red blood cells (microcytes). As these mix with the existing normal-sized cells, the overall size variation increases, leading to a high RDW. Other nutrient deficiencies, such as a lack of Vitamin B12 or folate, are also very common causes.
How often should I get my Red Cell Distribution Width (RDW) tested?
RDW is a standard part of a Complete Blood Count (CBC), which is one of the most frequently ordered lab tests. For healthy individuals, a CBC may be performed as part of a routine annual physical. If you have a chronic condition like heart disease, kidney disease, or a previously diagnosed anemia, your doctor may order a CBC more frequently (e.g., every 3-6 months) to monitor your condition and your response to treatment.
Can lifestyle changes improve my Red Cell Distribution Width (RDW) levels?
Yes, absolutely. Since high RDW is often a reflection of underlying nutrient deficiencies or chronic inflammation, lifestyle changes can have a significant impact. Correcting an iron, B12, or folate deficiency through diet or supplementation (as directed by a doctor) can directly normalize RDW. Furthermore, adopting an anti-inflammatory diet, engaging in regular exercise, managing stress, and quitting smoking can reduce the systemic inflammation and oxidative stress that contribute to a high RDW, thereby improving red blood cell health and lowering the value over time.
Medical Disclaimer
This article is for educational purposes only. Always consult a healthcare professional.